The brain and nerve system are both affected by the uncommon and deadly hereditary condition known as fatal familial insomnia (FFI). Being a prion illness, it is brought on by an aberrant version of the protein prion protein,...
The brain and nerve system are both affected by the uncommon and deadly hereditary condition known as fatal familial insomnia (FFI). Being a prion illness, it is brought on by an aberrant version of the protein prion protein, which builds up in the brain and harms nerve cells.
FFI commonly strikes individuals in their 40s or 50s and advances quickly, often resulting in death a year or two after the beginning of symptoms. Progressive sleeplessness, which is frequently the first symptom to manifest, is a characteristic of the illness. This is followed by a variety of neurological symptoms, such as hallucinations, dementia, and mobility abnormalities.
A mutation in the PRNP gene results in FFI, a hereditary disorder. As a result of the disease's autosomal dominant inheritance pattern, a person only has to inherit one copy of the mutant gene from one parent to become ill.
FFI has no known therapy; instead, supportive care is provided with the goal of symptom relief and patient comfort. There is optimism that new medicines will one day be created thanks to continued research into the illness.
A genetic anomaly with deadly consequences: the fascinating story of fatal familial insomnia
Italian neurologist Dr. Ignazio Roiter initially coined the term fatal familial insomnia (FFI) in the 1980s. In the Veneto area of Italy, Roiter noticed a family that had an odd pattern of sleeplessness that appeared to run in the family. The family members' sleeplessness would get increasingly worse, which would cause a variety of neurological problems and, eventually, death.
When a family in the United States was discovered to have FFI in the 1990s, the illness garnered worldwide Urine Routine notice. The fact that the family might be linked to an ancestor who lived in the 18th century suggests that the illness has run in the family for many generations.
However, there is still a great deal to learn about FFI and research into the condition is still being done today in the hopes of creating efficient cures and treatments.
The genetic puzzle of fatal familial insomnia: unraveling its causes
- A change in the PRNP gene, which produces the prion protein, results in FFI.
- The mutated prion protein, known as PrPSc, develops as a result of the mutation.
- A pathogenic agent called PrPSc causes additional PrPSc to misfold into more normal prion protein, which builds up in the brain.
- The symptoms of FFI are brought on by the buildup of PrPSc, which results in the deterioration of brain tissue and nerve cells.
- Because FFI is an autosomal dominant genetic disorder, it can only be passed down from one parent who has one copy of the defective gene.
The illness is not infectious and cannot be spread by exposure to body fluids or any other methods.
From restless nights to complete exhaustion: the signs and symptoms of fatal familial insomnia
There are four phases to the signs and symptoms of fatal familial insomnia (FFI):
Stage 1: Anxiety and insomnia
- Having trouble falling and staying asleep
- Anxiety, agitation, and panic episodes getting worse
- excessive perspiration and a rapid heartbeat
- Fatigue and loss of weight
Stage 2: Phobias and hallucinations
- development of hallucinations, frequently affecting the senses of sight and hearing
- Worsening of agitation and anxiety
- beginning of phobias, such as a fear of loud or light
Stage 3: Motor disturbances and dementia
- cognitive function has significantly deteriorated, resulting in memory loss, confusion, and disorientation.
- severe coordination issues, balance issues, and mobility issues
- Speech slurring, swallowing issues, and twitching of the muscles
Stage 4: Complete slumber and dementia
- total inability to sleep, which results in weariness and a decline in physical and mental health
- inability to recognize or converse with loved ones
- complete loss of motor and cognitive control
- Death often happens 12 to 18 months after symptoms first appear.
It's crucial to remember that the course of FFI can differ from person to person and that not everyone will experience all of the symptoms or move through all of the stages of the illness.
When the brain fails to Rest: exploring the Pathophysiology of fatal familial insomnia
The buildup of an aberrant form of the prion protein (PrPSc) in the brain is associated with the pathophysiology of fatal familial insomnia (FFI). The following are the main elements of FFI's pathophysiology:
Protein Folding
PrPSc buildup results from aberrant prion protein folding, which is caused by the defective PRNP gene. PrPSc builds up in certain regions of the brain, including the thalamus, which controls sleep and other vital processes.
Neurodegeneration
A buildup of PrPSc causes the brain's nerve cells, particularly those in the thalamus, to deteriorate. As a result, there is a steady decline in brain activity and the typical signs of FFI.
Protein buildup
The buildup of PrPSc in the thalamus, which is essential for controlling sleep-wake cycles, disturbs these cycles and causes sleep disturbance. The sleep problems that characterize FFI's early stages and finally lead to full insomnia are brought on by this.
Cognitive decline
As the illness worsens, the buildup of PrPSc in the brain causes extensive nerve cell destruction, which results in cognitive decline Urine Culture and dementia. This is because brain tissue is being destroyed and vital brain functions that are required for memory, thinking, and other cognitive processes are being lost.
In addition to impairing cognition, the buildup of PrPSc in the brain also results in motor dysfunction, which manifests as issues with coordination, twitching muscles, and difficulties speaking and swallowing.
When family history is a clue: diagnosing fatal familial insomnia
FFI is a condition that is highly rare and has certain symptoms in common with other neurological conditions, making a diagnosis difficult. The following are some of the main methods for diagnosing FFI:
Genetic testing
Since the PRNP gene mutation causes FFI, genetic testing can be utilized to confirm the diagnosis of the condition. The test can pinpoint the precise mutation in the PRNP gene linked to FFI, and it may be used to evaluate whether a patient's relatives are also at risk of contracting the illness.
Clinical assessment
A clinical assessment can be performed to gauge the disease's symptoms and course. This may entail a medical CSF Examination Routine examination, neurological tests, and memory-testing cognitive evaluations.
Polysomnography:
Sometimes referred to as sleep studies, is a technique used to assess and identify sleep problems, such as fatal familial insomnia (FFI). A patient is attached to many devices during a sleep study that racks their heart rate, respiration, brain waves, and other physiological processes.
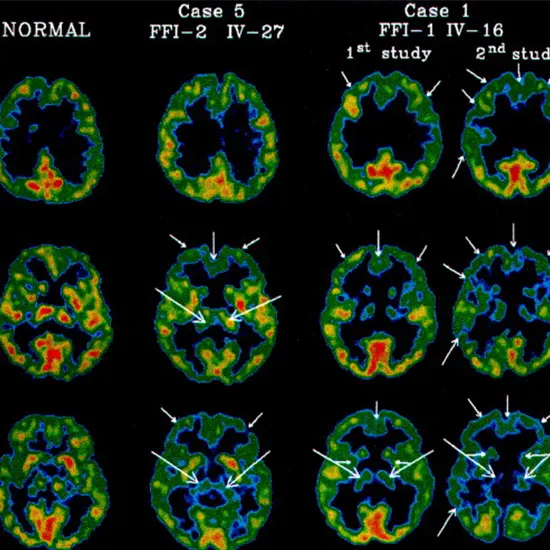
Imaging Studies
The diagnosis of fatal familial insomnia (FFI) may be aided by the use of brain imaging methods like positron emission tomography (PET) and magnetic resonance imaging (MRI). These examinations enable medical professionals to examine the composition and operation of the brain and spot any anomalies that could point to FFI.
Overall, a combination of clinical evaluation, family history, genetic testing, sleep studies, and brain imaging may be used to diagnose FFI and rule out other conditions that can cause similar symptoms.
A disease without a cure : exploring the treatment options for fatal familial insomnia
Sadly, there isn't a treatment for fatal familial insomnia (FFI) at the moment. The goal of treatment is to MRI Spectroscopy manage symptoms and enhance the patient's quality of life by offering supportive care. Here are some strategies for treating FFI symptoms:
Medication
Patients with FFI may benefit from using benzodiazepines and other sedative medications to treat their anxiety and sleeplessness.
Nutrition support
As FFI worsens, patients may lose weight and become undernourished. A feeding tube or intravenous nourishment can be given to the patient to ensure they are getting enough to eat.
Management of other symptoms
Patients with FFI may also develop dementia, speech and mobility issues, hallucinations, and other symptoms. Medication and other supportive measures may be used to treat these symptoms.
Palliative care
In the later stages of FFI, palliative care may be given to patients to better their quality of life while managing pain and other symptoms.
It's critical to remember that FFI has a terrible prognosis, with a median survival span of only 18 months from the beginning of symptoms. Therefore, CBC rather than trying to find a cure, the emphasis of treatment is on treating symptoms and offering comfort.
Defeating fatal familial insomnia: the battle begins with us.









