The first description of mammary analog-secreting carcinoma (MASC) was by Skalova et al. Since then, he has reported more than 70 cases, often in small batches of 10 or less.
The first description of mammary analog-secreting carcinoma (MASC) was by Skalova et al. Since then, he has reported more than 70 cases, often in small batches of 10 or less.
MASC can occur anywhere in the head and neck region, however it is most commonly found in the parotid region. Children and young adults are among the patients, who range in age. Low-grade MASC is regarded as such. But there have been reports of sophisticated metamorphosis and combative clinical behaviour.
Although the prognostic significance of MASC is not yet clear, there is evidence that MASC has a prognosis comparable to other (low-grade) salivary gland tumors. MASC is a small tumor, usually a few centimeters in diameter.
Clinical/radiographic features include a description as an isolated tumor mass with partly cystic structures and well-defined boundaries, comparable to a secretory carcinoma of the breast.
Interpretation of MASC histologically as pleomorphic adenoma, mucoepidermoid carcinoma, adenocarcinoma not specified (NOS), low-grade salivary gland carcinoma or acinic cell carcinoma (ACC) is a common and erroneous therapeutic approach. may lead to Similar to the genetic profile Ultrasound FNAC of secretory breast cancer, distinct genetic alterations have been reported for MASC, an ETV6-NTRK3 gene fusion with a translocation. However, his ETV6 rearrangements with fusion partners other than NTRK3 have recently been reported.
These translocations are usually not present in other salivary gland tumors and may help establish a correct diagnosis. In order to prevent MASC from becoming a diagnostic trap, particularly in tiny samples of salivary MR Spectroscopy gland tumours, this paper covers three instances that have been thoroughly characterised immunohistochemically and discussed in terms of differential diagnosis.
Materials and Methods
Patient samples and clinical data.
Three patients with primary diagnosis of MASC was included. In this study, the diagnosis of MASC was reviewed by independent consultant pathologists who are experts in the field of salivary gland MRI Both Breasts pathology. According to the Helsinki Declaration, this study has received approval from the regional ethics committee (No. 212108). Each patient provided their informed permission.
Fluorescence in situ hybridization.
The manufacturer's procedure was followed while using ETV6 Dual Colour Break Apart probes for fluorescence in situ hybridization (FISH) from ZytoVision, Bremerhaven, Germany. Zeiss AxioScope fluorescent Breast Ultrasound microscope with 10x and 63x oil objectives was used to study hybridised slides. We checked 100 randomly chosen non-overlapping tumour cell nuclei for the existence of colocalization (yellow) or translocation signals (green and red).
Result
Clinical and follow-up data
This study included 3 MASCs treated with Klinikum Rechts der Isar (Munich, Germany) and HNO-Klinik (Lübeck, Germany), including 2 male and 1 female patients. rice field. The patient's age ranged from he was 34 to he was 74. The tumor was located in he one of the parotid regions.
C2 and C3) or the floor of the mouth from the minor salivary glands (C1). Interestingly, one case of parotid MASC was localized near an additional pleomorphic adenoma (C2). Clinical manifestations depend primarily on tumor location.
Both parotid instances had a past history of tumours lasting up to a year, along with swelling (either painful or not). A mucosa-associated tumor nodule at the floor of the mouth caused increased pain and was resected 1 month after the onset of pain.
All of the lesions were pT1 tumors that ranged in size from 0.8 cm to 2.2 cm. The tumor was radically resected and in two cases additional neck dissection was performed at the ipsilateral level (C1:For Levels I-III, C3: Stage IV) has been implemented. No adjuvant therapy was used. All patients were followed up and were free of locoregional recurrences and metastases (up to 26 months).
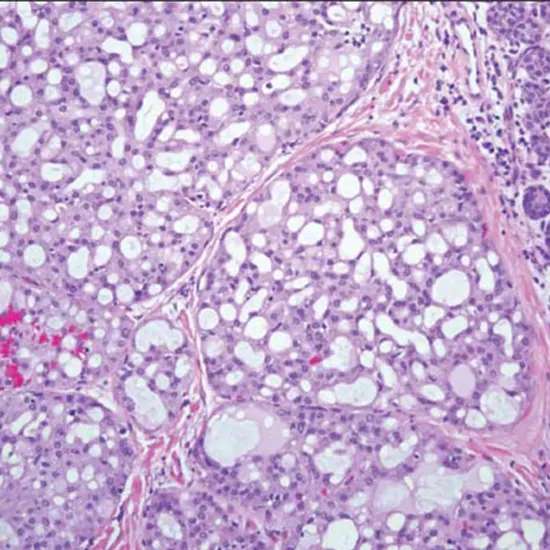
All three tumors exhibited a characteristic morphological pattern.
Well sealed, composed of epithelial lesions arranged in tubular and tubular cystic, papillary, and cribriform structures, with foamy histiocytes and copious intraluminal (alcian-PAS-positive) secretions There may be at least partially encapsulated tumor nodules.
Tumor cells have low cellular pleomorphism, moderate cell size, oval to round nuclei, and mostly polygonal, eosinophilic cytoplasm and focally vacuolated nucleoplasm. increase. Indicated. No or very few typical mitosis were observed. No necrotic areas could be detected. There Mammography X-Ray were no diastase-resistant PAS-positive granules. All tumours displayed significant CK7 staining and moderate to strong mammaglobin and S100 positivity, according to immunohistochemistry. In addition, all cases showed focal positivity for CK5/6 and two cases showed moderate to strong positivity for muc-4.
Proliferation was calculated to be up to 10% (C1:5%, C2:10%, C3:five percent). CK14, hormone receptors (estrogen and progesterone receptors), Her2/neu, p53, prostate-specific antigen (PSA), and androgen receptor (AR), on the other hand, consistently revealed negative results in all three cases.
Discussion
His MASC of the salivary glands is a distinct new entity recently described and just established in the new WHO classification of head and neck cancers (4th edition, 2017). We present three cases of MASC that have typical ETV6 rearrangements and display a homogeneous immunohistochemical profile including strong positivity for CK7, S100, partial muc-4, and mammaglobin.
Interestingly, no expression of hormone receptors [estrogen (ER) and progesterone (PR) receptors] or Her2/neu was detected, as previously described in the literature. Her2/neu over [removed] or Her2/neu gene amplification) is controversial as a potential therapeutic option for secretory breast cancer corresponding to her MASC of the breast.
Therefore, focal positivity of CK5/6 in MASC combined with negativity for hormone receptors and Her2/neu may indicate its more basal phenotype. Because of its eosinophilic and partially cystic appearance with the formation of glandular and tubular structures, MASC is easily misinterpreted, especially in small biopsies.
Different grades of benign and malignant salivary gland tumors are among the most important differential diagnostic considerations, so it is important to consider even a small biopsy for the correct diagnosis.
Among the most common salivary gland tumors that mimic MASC are pleomorphic adenoma, mucoepidermoid carcinoma, acinic cell carcinoma, salivary duct carcinoma, and unspecified adenocarcinoma. MASC can readily mimic pleomorphic adenoma (PA) both clinically and histologically.
The main causes of the misleading diagnosis of PA are:
i) Often a well-defined growth pattern of MASC.
ii) Histological appearance of tubular cysts and diffuse S100 positivity.
However, pleomorphic adenomas have been described as negative for these markers, thus staining for mammaglobin and/or muc-4 can reliably rule out PA. Mucoepidermoid carcinoma may be misdiagnosed because MASC may be focally positive for CK5/6, mimicking the typical squamous foci of mucoepidermoid carcinoma.
However, mucus cells, a key finding in mucoepidermoid carcinoma, are absent in MASCs. In addition, most mucoepidermoid carcinomas harbor specific translocations of her MAML2) locus like a mastermind.
Acinic cell carcinoma, possibly the most typical MASC misinterpretation, is distinguished by diastase-PAS-resistant zymogen granules and an immunohistochemistry profile that includes negative staining for mammaglobin and S100. MASC cases with more apocrine manifestations can be distinguished from salivary ductal carcinoma by immunohistochemical staining for androgen receptor, PSA, and Her2/neu.
Finally, the diagnosis of otherwise unspecified adenocarcinoma (adenocarcinoma NOS) is a diagnosis of exclusion, these tumors are high-grade neoplasms and biopsy diagnosis warrants a more aggressive therapeutic approach. can cause it and should be evaluated carefully.
However, if the immunohistochemical profile is inconsistent, FISH analysis of ETV6 locus rearrangements can help to correctly diagnose MASC. Based on the literature to date, the ETV translocation appears to be MASC-specific. Since persistent pleomorphic adenoma was an unknown finding in his MASC, the physician should be aware that multinodular lesions of the salivary glands may carry two different entities.
Conclusion
In summary, MASCs are molecularly defined key units of the salivary gland that may be low-level malignancies in most cases reported to date.An accurate diagnosis can help shed further light on this novel type of potentially low-grade salivary gland tumour and is crucial for the selection of the most effective course of action.









