One of the most frequent causes of preventable blindness in developing countries is trachoma. It was named as one of the seven most prevalent tropical illnesses that are treatable with drugs.
One of the most frequent causes of preventable blindness in developing countries is trachoma. It was named as one of the seven most prevalent tropical illnesses that are treatable with drugs. Most often, those who live in areas without access to clean water or basic sanitary facilities are its victims.
Trachoma is believed to be the principal cause of vision impairment in over 2.2 million people worldwide, including roughly 1.2 million people who are completely blind. The SAFE (surgical, antibiotics, facial cleaning, and environmental management) method has significantly decreased the incidence of trachoma, thanks in part to assistance from the International Trachoma Initiative (ITI).
The word "trachoma" is a Greek word that means "roughness."
It was generally known and recognised that trachoma was a "ophthalmia".
According to Taborisky and MacCallan, the origin of this disease is believed to be in Central Asia.1, 2 The Hippocratic Corpus, which dates back to 1600 A.D., as well as various other medical writings, and 1700 A.D.2 In the Egyptian War, military operations aided Napoleon's troop expansion by blinding many.
Between 1200 and 1500 A.D., trachoma was common in Europe.
Three thousand people contracted "Egyptian military ophthalmia" in 1798, and the European trachoma epidemic was sped up by the Napoleonic Wars.2
To stop the spread of contagious eye disease, British researchers B.C.) (40-91 A.D.), and Galen suggested cleanliness, isolation, and better living circumstances for soldiers in 1810.
International organisations joined forces to fight trachoma because of its global dispersion. The International Organisation against Trachoma and La Liege Contre Le Trachoma were established prior to World War II. Additionally, trachoma was designated a hazardous disease for humans by the World Health Organisation (WHO) shortly after its founding.
Pathogenesis
The bacterium Chlamydiae must live inside cells. Serotypes A, B, and C of Chlamydia trachomata’s are responsible for trachoma. Chlamydia infection of the ocular surface results in a chronic inflammatory response that is marked by the presence of lymphocytic, monocytic, plasma cells, and macrophage infiltrates.
As a result of chronic and recurring conjunctival follicular reinfection, prolonged inflammation causes conjunctival scarring.11, 12 Chlamydial infections cause the conjunctival epithelium's regular architecture Ultrasound B Scan to be altered, the goblet cells to disappear, and the typical, loose, vascular sub-epithelial stroma to be replaced by compact bands of type IV and type V collagen.
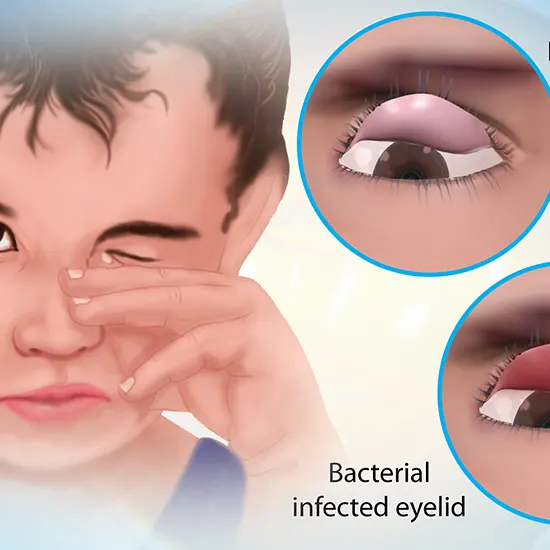
The keratoconjunctivitis known as trachoma is mucopurulent. In the upper palpebral conjunctiva, there is an inflammatory and follicular reaction. C. trachomata’s can potentially infect extra ocular mucous tissues including the nasopharynx. The diagnosis appears to be supported by common clinical symptoms in an endemic region.
To confirm the diagnosis, however, laboratory testing are required. The diagnosis of trachoma has been made possible by a number of various laboratory tests. In low prevalence areas or for study, these tests are Giemsa Stain helpful for diagnosis. The intracytoplasmic inclusions of C. trachomatis can be found using cytologic procedures such as Giemsa staining14 or direct fluorescent antibody (DFA) tests15.
Clinical presentation
As was previously mentioned, trachoma can be diagnosed based on the clinical signs and symptoms present in endemic regions.
Inclusion conjunctivitis, viral conjunctivitis, bacterial conjunctivitis, and allergic conjunctivitis are all possible differential diagnoses for trachoma.
The most frequent reason for red, itchy eyes is allergic conjunctivitis. There may also be insufficient mucosal discharge and a papillary reaction on the conjunctiva. The symptoms of viral conjunctivitis Direct Immunofluorescence include burning eyes and a feeling of a foreign body. On inspection, tender pre-auricular lymph nodes may also be visible.
A history of an upper respiratory tract illness may be mentioned by the patient. In trachoma, this is not typically present. A purulent discharge is the defining characteristic of bacterial conjunctivitis. Follicular conjunctival reaction is less common than trachoma.
Follicular trachoma
is defined by the presence of at least five follicles on the central portion of the upper tarsal conjunctiva, each of which must be at least 0.5 mm in diameter. The existence of follicles is thought to be a sign of a disease that is active. Most frequently, TF is observed in kids between the ages of 3-5. Lymphocytes are gathered in thick follicles. Herbert pits are depressions that can develop as a result of involution of limbal follicles. These lesions are diagnostic of trachoma that was formerly active.
Trachomatous inflammation-intense (TI)
is a severe inflammatory thickening and papillary enlargement of the upper tarsal conjunctiva that obscures more than half of the typical deep tarsal veins. After TI, there is a higher chance of developing serious conjunctival scarring and a blinding condition.
Trachomatous scarring (TS)
is a condition in which the tarsal conjunctiva has white bands, lines, and sheets of fibrosis. Trichiasis and dry eye condition are both correlated with TS, a marker of previous inflammatory illness.
Corneal opacity (CO):
is identified by the existence of prominent corneal opacity across the pupil. Through the opacity, the pupillary edge is obscured. The CO stage of trachoma causes blindness. Opacity comprises infiltration, pannus, and epithelial vascularisation.
Management and prevention
To direct global efforts to eradicate this blinding illness, the WHO promoted a trachoma prevention and treatment strategy. Primary, secondary, and tertiary prevention are the three components that make up the "SAFE" public health strategy. The SAFE method has been shown to be extremely beneficial for treating and preventing trachoma. The parts of SAFE are as follows:
Environmental advances; surgery; antibiotics; facial cleanliness;
To assist in achieving the WHO's goal of eradicating blinding trachoma by 2020, the International Trachoma Initiative (ITI) was established in 1998. The SAFE strategy for trachoma control is being implemented by ITI in partnership with governmental and nongovernmental organisations at the local, national, and worldwide levels.
Surgery
Surgery is done to turn the eyelashes inward in patients with trichiasis or entropion, and is crucial to avoid blindness. It is an easy treatment that can be easily completed at medical facilities or in the community. Typically, patients favour surgical procedures that may be completed in an outpatient setting.
Antibiotic therapy
By the 1950s and 1960s, trachoma had been eradicated in the majority of industrialised nations as a result of the introduction of antibiotics in the 20th century, which had a revolutionary effect on the disease's management. Infected population infection burden reduction or active disease treatment are the goals of antibiotic therapy.
Facial cleanliness
Children with filthy faces have a higher risk of contracting trachoma and passing it on to others if they are infected than those who are not. Ocular and nasal discharges encourage the growth and attraction of infectious flies, and touching filthy eyes with cloth, sheets, and mother's clothing, specifically shawls, aids in the spread of trachoma.
Environmental improvement
It has long been understood that trachoma prevalence is correlated with local resident living circumstances, access to clean water, and availability of proper sanitation.By raising residents' standards of living and providing a sufficient supply of clean water, trachoma transmission can be stopped at the community level.
Future directions
By 2020, blinding trachoma had to be completely eradicated worldwide, the WHO urged in 1998.41, 42 As was already mentioned, Iran is one of the nations that has announced the accomplishment of eradication goals in the Middle East and North Africa alongside Morocco and Oman.34 Trachoma, however, continues to be a public health issue in some parts of eastern Iran, despite numerous attempts to eradicate it, according to a recent report43.
Numerous explanations for their predominance have been put up, including interactions with Afghans, a lack of water, and dust storms in certain regions. It has been demonstrated that places with starvation, poor hygiene, and low living conditions have higher rates of trachoma.









