A sickle cell disease is a group of acquired red blood cell disorders that affect hemoglobin. More than 100,000 individuals in the United States and 20 million individuals globally are affected by this illness.
What is Sickle Cell Disease?
A sickle cell disease is a group of acquired red blood cell disorders that affect hemoglobin. More than 100,000 individuals in the United States and 20 million individuals globally are affected by this illness.
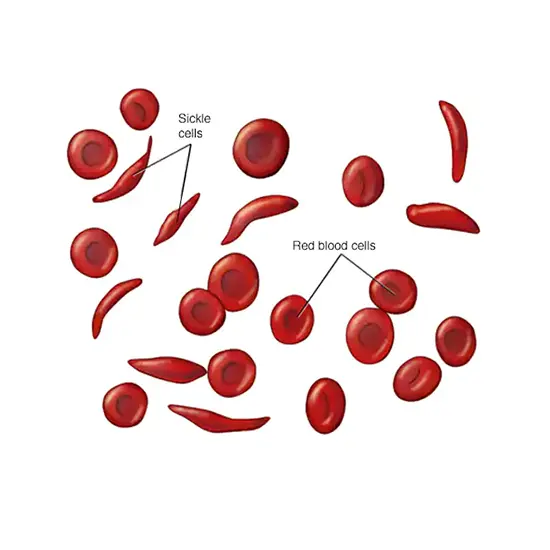
Red blood cells often have a disc shape and are malleable enough to pass through blood channels without difficulty. Your red blood cells will have a sickle or "sickle" form if you have sickle cell disease. These difficult-to-move, stiff cells can restrict blood flow to other body parts. Blocked blood flow in the body can lead to serious complications, including eye problems, stroke, infections, and pain known as attacks.
Sickle cell disease is a lifelong disease. Blood and bone marrow transplants are the only cure for this, but some treatments can relieve symptoms and prolong life. Your healthcare team will work with you on a treatment plan to relieve your symptoms and manage your condition.
How Frequent is Sickle Cell Disease?
The frequency section has been increased.
Millions of people worldwide are afflicted by sickle cell disease.
According to estimates, 1 in 500 African Americans and 1 in 1,000 to 1,400 Hispanic People will contract the illness.
Pathophysiology of Sickle Cell Disease
The pathophysiology of sickle cell disease is primarily characterized by the loss of red blood cell flexibility. Normal red blood cells can deform to pass through capillaries because they are quite elastic and have a biconcave disc shape. Low oxygen tension encourages red blood cell sickling in sickle cell disease, and repeated episodes of sickling harm the cell membrane and reduce cell flexibility. When the usual oxygen tension is restored, these cells do not regenerate. Due to their rigidity, these blood cells cannot bend as they go through tiny capillaries, which causes artery obstruction and ischemia.
Due to the structure of red blood cells, hemolysis—the death of the cells—causes the true anemia of the sickness. Red cell production by the bone marrow does not keep up with the pace of destruction, despite efforts to do so. Healthy red blood cells normally function for 90 to 120 days, but sickled cells only function for 10 to 20 days.
What Causes Sickle Cell Anemia?
The HBB gene is mutated in sickle cell disease. A fraction of hemoglobin is produced according to instructions from the HBB gene. Four protein subunits, typically two alpha-globin and two beta-globin, make up hemoglobin. The HBB gene contains information required to produce beta-globin. The HBB gene has undergone several mutations that result in various beta-globin variants. Hemoglobin S is a variant of beta-globin caused by a particular mutation in the HBB gene (HbS). Hemoglobin C (HbC) and hemoglobin E are further defective beta-globin variants. Low levels of beta-globin can also result from mutations in the HBB gene; this condition is known as beta-thalassemia.
Hemoglobin S is used in place of at least one beta-globin component in individuals with sickle cell disease. In sickle cell disease (also called pheochromocytomas). Hemoglobin S replaces two beta-globin subunits in the most prevalent form of sickle cell disease, homozygous sickle. Hemoglobin S replaces one of the beta-globin subunits of hemoglobin in various forms of sickle cell disease. Another aberrant variation, such as hemoglobin C, is used to replace the other beta-globin component. For instance, individuals with sickle cell disease C (HbSC) have hemoglobin molecules that substitute beta-globin for hemoglobin S and hemoglobin C. People have hemoglobin S-beta-thalassemia if the mutations that cause hemoglobin S and beta-thalassemia co-occur (HbS Beta Thal).
Beta-globin variants that are abnormally formed can give red blood cells a sickle shape. Inactive sickle cells can occasionally become lodged in tiny blood channels, which can have life-threatening consequences.
What are the Signs and Symptoms of Medical Conditions Linked to Sickle Cell Anemia?
Usually, appear around 6 months of age. They are different for each person and can change over time. Signs and symptoms include:
- Anemia- Sickle cells are easily destroyed and die. Red blood cells have a life of 120 days before needing replacement. However, sickle cells usually die in 10 to 20 days, resulting in anemia. Due to the lack of RBCs body can’t get enough oxygen, which leads to fatigue.
- Pain episodes- The primary symptom of sickle cell anemia is recurrent episodes of pain, sometimes known as pain crises. Pain occurs when crescent-shaped red blood cells travel through small blood vessels and block blood flow to the chest, abdomen, and joints. The pain can vary in intensity and last from hours to days. Some people experience pain only a few times a year. Others have a dozen or more per year. Severe pain attacks require hospitalization.
Some teenagers and adults with sickle cell disease have chronic pain due to bone or joint damage, ulcers, or other causes. Swelling of limbs. The swelling is caused by crescent-shaped red blood cells blocking blood flow to the limbs.
- Several infections- The spleen may suffer damage from sickle cell disease and become more prone to infections. Antibiotics and immunizations are frequently given to infants and kids with sickle cell disease to help them avoid potentially fatal illnesses like pneumonia.
- Puberty or retarded growth- The body gets the oxygen and nutrition it needs from red blood cells to flourish. Infants, toddlers, and teenagers may experience slowed growth and delayed puberty due to a shortage of healthy red blood cells.
- Eyesight issues- The tiny blood arteries that supply the eye can become blocked by sickle cells. The retina, the area of the eye that processes visual images, may be harmed as a result, impairing vision.
When to See a doctor
See your doctor right away if you or your child have symptoms of sickle cell anemia. Children with sickle cell anemia are susceptible to infections, often beginning with a fever, which can be life-threatening, so if her fever is over 100°F (38.5°C), see a doctor immediately.
See emergency care for symptoms of stroke, such as:
- One side of the face, a leg, or an arm may be paralyzed.
- Confusion
- Difficulty walking or speaking.
- Sudden change in vision
- Unexplained hearing loss
- Severe headache
"Unforeseen Challenges Arise: Navigating the Complexities of a Situation"
Sickle cell disease can lead to a variety of complications, including:
- Stroke: Sickle cells can prevent blood from reaching a specific part of the brain. Seizures, numbness or weakness in the arms and legs, garbled speech that appears out of nowhere, and loss of consciousness are all indications of a stroke.
- Chronic chest syndrome: This potentially fatal complication can result from a lung infection or sickle cell anemia, which blocks the blood veins in the lungs and causes chest discomfort, fever, and shortness of breath.
- Pulmonary arterial hypertension: People with sickle cell anemia may have high blood pressure in the lungs. This complication usually affects adults.
- Spleen confinement: large numbers of sickle cells can become trapped in the spleen, causing the spleen to enlarge and possibly causing stomach-ache. It can be life-threatening. Guardians of children with sickle cell anemia ought to routinely feel their child's spleen expanding. blind. Sickle cells can block the small blood vessels that supply the eye. May result in blindness over time.
- Foot ulcers: Legs can develop painful open sores as a result of sickle cell anemia. Gallstones. Bilirubin is a by-product of red blood cell decomposition. Gallstones can develop if bilirubin levels are too high in the body.
- Sexualism: Men with sickle cell anemia may feel pain and protracted erections in this situation. Sickle cells may obstruct the penis's blood vessels, which over time may result in impotence.
- Deep vein thrombosis: Sickle cell disease of the red blood cells can cause blood clots, increasing the risk of blood clots getting stuck in the deep veins (deep vein thrombosis) or lungs (pulmonary embolism).
- Complications during pregnancy: Sickle cell anemia can increase the risk of hypertension and blood clots during pregnancy. Premature birth, low birth weight, and miscarriage are additional risks that may be increased.
Treatment of Sickle Cell Anemia
- Penicillin and folic acid
Because of their underdeveloped immune systems, which make them more susceptible to early childhood infections, penicillin is advised to be taken daily from birth to age five.
The WHO had previously advised folic acid dietary supplements.
- Malaria avoidance
When infected with malaria, there may be a benefit to having sickle cell anemia disease (A) as opposed to a normal blood cell response (B).
Those with sickle cell illness are not protected by the sickle cell trait; in fact, this makes them more susceptible to malaria, which is the most prevalent cause of excruciating crises.
- Vaso-occlusive crisis
Vaso-occlusive crises, which are excruciatingly painful episodes, are the most common symptom of sickle cell disease. Nonetheless, there is a wide range in the occurrence, gravity, and length of these crises. Pain management calls for opioid drug administration at regular intervals until the crisis has passed. Painful crises are treated symptomatically with painkillers. A portion of patients manages NSAIDs for lesser crises (such as diclofenac or naproxen). Most patients need inpatient care for intravenous opioids for more serious situations.
- Stroke mitigation
Children with sickle cell anemia who are at high risk for stroke might be found using transcranial Doppler ultrasound (TCD). Because blood flow velocity is inversely proportional to arterial diameter and high blood flow rates are therefore indicative of blood vessels that are partially occluded by sickle cells, the ultrasound test can identify these blood vessels.
- Acute chest syndrome
The treatment is identical to vaso-occlusive crises with the addition of oxygen supplementation for hypoxia, close observation, and antibiotics (often a quinolone or macrolide, since cell wall-deficient ["atypical"] bacteria are thought to contribute to the illness). As of 2019, there is no standard antibiotic treatment because there is a lack of credible research on the effectiveness of antibiotics for acute chest syndrome in sickle cell disease patients. It is advised that patients with suspected acute chest syndrome be hospitalized, with worsening A-a gradient serving as a recommendation for ICU admission.
- Hydroxyurea
There is presently inadequate information to determine whether hydroxyurea, commonly known as hydroxycarbamide, reduces the frequency of painful episodes.
- Blood transfusion
Blood transfusions are frequently used to treat sickle cell disease in severe cases and to avoid complications by reducing the number of sickle-forming red blood cells (RBCs) by incorporating healthy red blood cells. When transcranial Doppler ultrasonography reveals aberrant cerebral blood flow in children, prophylactic RBC transfusion therapy has been demonstrated to lower the incidence of first stroke or silent stroke. It also lowers the incidence of subsequent silent strokes and recurrent strokes in people who have already experienced one.
- Bone marrow transplant
The only treatment for SCD that has been shown helpful in children is a bone marrow transplant. [106] Yet, due to the precise HLA type required, bone marrow transplants are challenging to obtain. The bone marrow required for the transplant would ideally come from an unrelated donor (allogeneic). Some gene therapies are being developed that would modify the patient's bone marrow stem cells outside of the body. These modified cells could then be transplanted back into the patient after chemotherapy kills the original, unaltered cells.
- Vascular death
The goal of treatment for sickle cell disease patients who have avascular necrosis of the bone is to lessen or stop the pain while maintaining joint mobility.
Resting the joint, physical therapy, painkillers, joint replacement surgery, or bone grafting are some of the current therapeutic options. To evaluate the best course of treatment and determine whether a combination of physical therapy and surgery is more successful than physical therapy alone, high-quality, randomized, controlled trials are required.
- Psychological therapies
Further study is needed to assess the efficacy of psychological therapies such as patient education, cognitive therapy, behavioral therapy, and psychodynamic psychotherapy that aim to supplement existing medical treatments.
"Though sickle cell disease presents significant challenges, ongoing research and advancements in treatment provide hope for a brighter future for those affected by this condition."









