The spirochete bacterium Leptospira interrogans is the source of the bacterial illness known as leptospirosis. It can be spread from animals to people since it is a zoonotic illness. The illness is mainly prevalent in...
The spirochete bacterium Leptospira interrogans is the source of the bacterial illness known as leptospirosis.
It can be spread from animals to people since it is a zoonotic illness. The illness is mainly prevalent in tropical and subtropical areas, where it is frequently accompanied with floods and a lot of rain.
Contact with polluted water, dirt, or the urine or other body fluids of infected rodents, cattle, pigs, or dogs can Blood Culture result in the transmission of leptospirosis. Through scrapes and abrasions on the skin as well as mucous membranes including the eyes, nose, and mouth, the bacteria can enter the body.
Leptospirosis can be prevented by avoiding polluted water and soil, using protective gear and footwear, and maintaining excellent hygiene.
This article will give in-depth understanding of leptospirosis.
Unveiling the Mystery of Leptospirosis: A Historical Perspective
Leptospira species, which are common in the environment and may infect both humans and animals, are the source of the bacterial illness leptospirosis. The first time leptospirosis was identified as an illness affecting animals, mainly cattle, was in the late 1800s.
Leptospirosis in humans initially became known in Japan in the early 20th century, when it was known as Weil's sickness after the German doctor who originally characterised it.
Leptospirosis epidemics were reported in several locations of the world throughout the ensuing decades, notably in tropical and subtropical areas with subpar sanitation and hygiene.
Leptospirosis became a major health problem for both soldiers and civilians in the Pacific theatre of World War II, when it was linked to contact with polluted water and soil. The condition, known Ultrasound as "Japanese fever," was also encountered in war prisoners and forced workers in Southeast Asia.
The 1950s and 1960s saw a revolution in medicine with the development of leptospirosis vaccines and antibiotics.
In many parts of the world, especially in developing countries, leptospirosis is still a serious public health problem. It is connected to poverty, overcrowding, and poor sanitation.
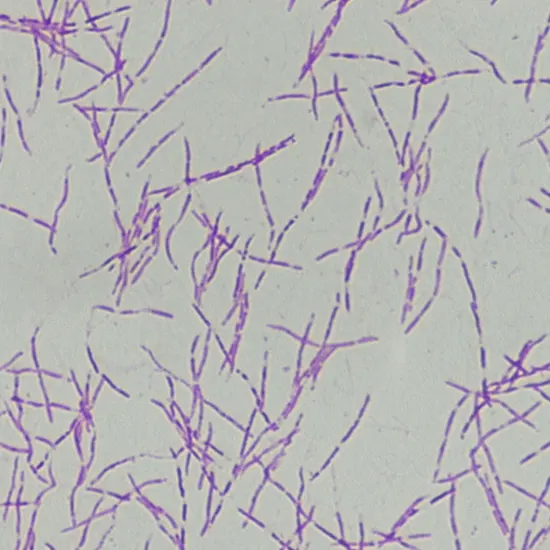
Exploring the Morphology of Leptotrichosis
The bacteria Leptotrichia buccalis, a gram-negative, anaerobic, non-spore-forming bacillus, is what causes leptotrichosis. The following are some noteworthy characteristics of this bacterium's morphology:
- Leptotrichia buccalis is a long, thin bacillus that is 2-3 m in length and 0.2-0.3 m in breadth.
- When stained with the Gramme stain, the bacteria exhibits pink coloration because it is gram-negative.
- Leptotrichia buccalis lacks flagella and is not able to move.
- The bacteria grows on agar medium in the form of tiny, transparent, non-pigmented colonies.
- Leptotrichia buccalis is an obligate anaerobe, which implies that it needs an oxygen-free environment to develop.
- The bacterium is a fermentative organism that results in the production of succinic acid and lactic acid as byproducts of fermentation.
- Leptotrichia buccalis can cling to the epithelial cells in the oral cavity, which increases the pathogenicity of the organism.
Leptotrichia buccalis has a general shape that is characteristic of an anaerobic, gram-negative bacillus, and its capacity to cling to host cells plays a role in its capacity to infect the oral cavity.
A Closer Look at Leptotrichosis: Exploring the Bacterial Life Cycle
Leptotrichia buccalis, the bacterium that causes leptotrichosis, does not have a distinct life cycle in the traditional sense, as it is a single-celled organism that reproduces by binary fission.
However, there are some key features of the bacterium's growth and behavior that can be considered part of its life cycle. Here are some of the salient features of the life cycle of Leptotrichia buccalis:
Growth and reproduction
Like all bacteria, Leptotrichia buccalis reproduces asexually by binary fission, which involves the division of one cell into two identical daughter cells.
Colonization
Leptotrichia buccalis is a commensal bacterium that is normally found in the oral cavity of humans, where it can live and grow without causing harm.
Pathogenesis
Under certain conditions, such as in the presence of other pathogenic organisms or in individuals with compromised immune systems, Leptotrichia buccalis can become pathogenic and cause disease.
Transmission
Leptotrichia buccalis is not typically thought to be very contagious from person to person, although it can be transmitted by direct contact with infected oral secretions or through contact with contaminated surfaces.
Antibiotics like penicillin or metronidazole can be used to treat Leptotrichia buccalis in order to get rid of the bacteria and stop the condition from spreading.
Leptotrichia buccalis's whole life cycle covers the bacterium's proliferation, colonisation, and possible pathogenesis in the oral cavity, as well as how it reacts to antibiotic therapy.
The Hidden Threat: Leptotrichosis and its Impact on Oral Health
The bacterium Leptotrichia buccalis causes leptotrichiasis, commonly referred to as leptotrichosis. The following are some key signs of leptotrichiasis infection:
Site
Leptotrichiasis typically affects the oral cavity, which includes the tonsils, tongue, and gums.
Symptoms
In addition to fever and malaise, the infection may result in symptoms including pain, swelling, and redness in the afflicted region.
Causative Agent
Leptotrichia buccalis is a commensal organism that is typically present in the human oral cavity. However, under specific conditions, such as following dental treatments or in people with weakened immune systems, it can turn pathogenic.
Risk factors
Poor oral hygiene, dental procedures, and immunosuppression are among variables that might raise the risk of leptotrichiasis.
Prognosis
Leptotrichiasis often has a fair prognosis and a self-limiting illness with quick and adequate treatment.
The overall condition of leptotrichiasis is a bacterial infection that mostly affects the oral cavity and can cause symptoms including pain, CT Scans swelling, and fever. It may be identified using molecular or culture-based techniques, and it can be treated with antibiotics.
The Diagnostic Dilemma: Identifying Leptotrichosis in a Sea of Oral Infections
The following are some methods for diagnosing leptotrichiasis:
Clinical presentation
The presence of the infection may be indicated by the leptotrichiasis symptoms, which include discomfort, swelling, and redness in the oral cavity.
Microscopic examination
Leptotrichia buccalis' distinctive long, thin, gram-negative rods can be found by looking for them under a microscope on a sample of the afflicted tissue.
Bacterial culture
To isolate and identify the bacteria, a sample of the Urine Culture afflicted tissue can be grown on the right medium.
Molecular detection
Leptotrichia buccalis DNA can be found in the afflicted tissue using polymerase chain reaction (PCR) methods.
Serological testing
Blood tests can be used to find anti-Leptotrichia buccalis antibodies, albeit they are not frequently accessible.
A early and accurate diagnosis is essential for the infection to be adequately treated and controlled.
Putting the Pieces Together: Tailoring Treatment for Leptotrichosis Infection
The following techniques can be used to treat leptotrichiasis:
Antibiotics
Antibiotics are the cornerstone of leptotrichiasis therapy. The bacteria is resistant to several drugs, including penicillin, Urine Routine metronidazole, clindamycin, and tetracycline. The length of the antibiotic therapy might range from a few days to a week, depending on how severe the infection is.
Supportive treatment
In addition to medications, managing the symptoms of the illness may call for supportive care including pain reduction and temperature control.
Surgical intervention
To remove contaminated tissue in severe instances of leptotrichiasis, surgical intervention such as abscess draining may be required.
Management of underlying disorders: Immunosuppression, poor oral hygiene, and dental operations are a few examples of underlying diseases that might contribute to leptotrichiasis. Taking care of these underlying issues can aid in preventing the infection from returning.
Leptotrichiasis is often treated with medicines, supportive care, and, if necessary, surgical intervention. Depending on the infection's severity and any underlying issues that could be fueling it, a particular treatment strategy will be chosen.
Don't Let Leptotrichosis Win: Stand Up and Fight for Your Oral Health.









