The cancer neuroblastoma arises from neuroblasts, which are immature nerve cells. The adrenal glands, which are situated above the kidneys, are where it often manifests, although it can also form in other body parts including...
Understanding Neuroectodermal Tumor: Neuroblastoma - with causes, symptoms, and Treatment plan.
An Outline
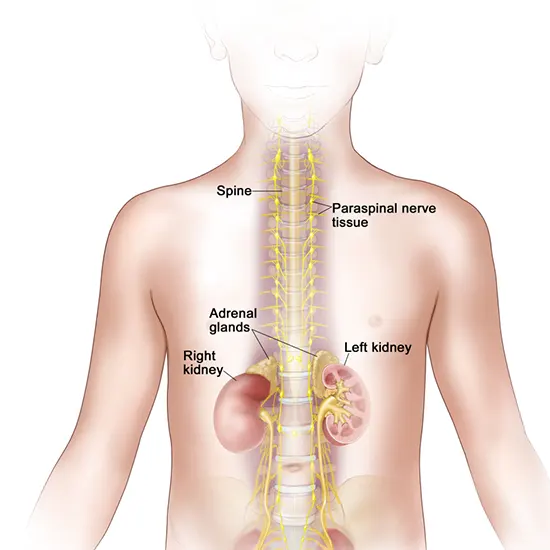
The cancer neuroblastoma arises from neuroblasts, which are immature nerve cells. The adrenal glands, which are situated above the kidneys, are where it often manifests, although it can also form in other body parts including the chest, neck, or pelvis.
Symptoms of neuroblastoma can vary depending on the location of the tumor, but they can include abdominal pain, weight loss, and a lump or mass in the affected area.
Treatment for neuroblastoma depends on the stage of cancer and the age of the patient. It may include surgery, chemotherapy, radiation therapy, and immunotherapy. The prognosis for neuroblastoma can also vary, with some patients being cured and others experiencing relapse or metastasis.
This article will shed light on the causes, symptoms, and treatment plans for neuroblastoma in detail.
Know The Commonness
Neuroblastoma is the most common cancer diagnosed in infants, and it accounts for around 6% of all childhood cancers. It is very rare in adults.
It is third on the list of cancers found in children after leukemia and brain tumors. The prevalence of neuroblastoma varies with age, with infants under the age of one experiencing the greatest rates.
The American Cancer Society estimates that there are roughly 800 instances of neuroblastoma identified in the US each year, with 90% of cases occurring before the age of five.
The prevalence of neuroblastoma is thought to be 1 in 7,000 children globally, with greater rates in specific places like Japan and Europe. Although the precise origins of neuroblastoma are not fully understood, environmental and genetic factors may be involved.
Known risk factors of neuroblastoma
Although the precise origins of neuroblastoma are not well known, several variables may support the growth of this malignancy. These elements consist of:
- Genetic mutations: The ALK, PHOX2B, and MYCN genes, which regulate cell growth and development, are often mutated in neuroblastoma. Normal cells may get malignant mutations that lead them to proliferate uncontrolled.
- Chromosomal abnormalities: A higher chance of developing neuroblastoma has been linked to chromosomal abnormalities, such as changes in the number or shape of chromosomes or the deletion of chromosome 1p.
- Environmental pollutants: Exposure to some environmental pollutants, such as pesticides or solvents, has been associated with a higher risk of neuroblastoma development.
- Genetic factors that run in families: Certain cases of neuroblastoma can be handed on from parents to their offspring through mutations in particular genes.
- Age: Since neuroblastoma most frequently affects young children, developmental factors could be involved in its development.
- Additional medical disorders: Neuroblastoma risk may be increased by several illnesses, including congenital abnormalities of the neurological system.
- Neural crest cell development: Neuroblastoma arises from neural crest cells, which are a type of embryonic stem cell that gives rise to the nervous system. Abnormal development of neural crest cells has been suggested as a potential cause of neuroblastoma.
- Epigenetic changes: Epigenetic changes, which alter gene expression without changing the underlying DNA sequence, have been found in neuroblastoma tumors.
- Immune system dysfunction: There is evidence that suggests immune system dysfunction may play a role in neuroblastoma development. For instance, some research has revealed that an increased risk of neuroblastoma may be linked to low amounts of certain immune cells.
- Hormonal variables: Hormonal factors have been proposed as potential risk factors for neuroblastoma, such as elevated levels of certain hormones.
Not all children who have these risk factors will acquire neuroblastoma, even though some of them have been linked to a higher risk of the illness. However, a lot of neuroblastoma cases don't have any identified risk factors, indicating that there could be other variables involved in the formation of the disease.
Know the body signals
The neuroblastoma signs and symptoms vary depending on the tumor's size, location, and whether or not it has metastasized (spread) to other body areas.
Typical neuroblastoma warning signs and symptoms include:
- Abdominal enlargement: One of the most typical symptoms of neuroblastoma, particularly in newborns and young children, is an abdominal enlargement or tumor. The swelling might be solid, asymmetrical, and painless.
- Pain: Children with neuroblastoma may have discomfort in their joints, bones, or abdomen.
- Fatigue: Weakness and weariness are common symptoms of neuroblastoma, especially if the tumor has progressed to the bone marrow.
- Fever: In younger children with neuroblastoma, a fever is a frequent sign of the disease.
- Hypertension: Neuroblastoma can result in hypertension, particularly in children with tumors that generate hormones.
- Anemia: Anemia, which can result in weakness, exhaustion, and a pale complexion, is a side effect of neuroblastoma.
- Tachycardia: Children with neuroblastoma may experience a quick heartbeat, also known as tachycardia, especially if the tumor is releasing hormones.
- Horner syndrome: When the tumor compresses neck nerves, an uncommon neuroblastoma symptom known as Horner syndrome develops. It can result in one side of the face not perspiring, drooping eyelids, and constricted pupils.
- Proptosis: If the tumor is close to the eye, it may cause bulging of the eye.
- Walking difficulties: If the tumor is close to the spinal cord, it may result in paralysis or difficulty walking.
- Seizures: Neuroblastoma tumors can occasionally lead to seizures, particularly if they have migrated to the brain.
- Swollen lymph nodes: Lymph nodes can swell and become sensitive when neuroblastoma is present, especially in the neck, chest, and groin.
- Weight loss: Despite having a healthy appetite, children with neuroblastoma may lose weight.
- Changes in bowel or bladder habits: Neuroblastoma can cause changes in bowel or bladder habits, such as constipation or incontinence.
- Irritability: Some neuroblastoma patients' behavior may change or they may become irritable.
- Bone pain: If the tumor has metastasized to the bones, discomfort, and soreness may be experienced.
- Breathing problems: If the neuroblastoma is close to the lungs or if it has spread to the lungs, it may be difficult to breathe.
- Bruising or bleeding: Neuroblastoma can lower platelet levels in the blood, which can result in bruising or bleeding.
It's crucial to remember that many of these symptoms are not exclusive to neuroblastoma. But if your child exhibits any of these signs, it's important to get them checked out by a doctor straight away.
Understanding the histological types
The prognosis and treatment options for neuroblastoma might vary depending on tumor type. The many varieties of neuroblastoma include:
- Favorable histology: Histologically, this kind of neuroblastoma has a better prognosis since tumor cells seem more developed and differentiated. These tumors have a decreased risk of recurrence and a tendency to develop more slowly.
- Unfavorable histology: Because tumor cells in this kind of neuroblastoma are more young and undifferentiated, the prognosis is less promising. These tumors often grow more quickly and have a higher risk of recurrence.
- Ganglioneuroblastoma: Both immature and adult nerve cells can be seen in this particular neuroblastoma. The prognosis is often excellent for ganglioneuroblastoma, which is atypically less aggressive than other forms of neuroblastomas.
- Ganglioneuroma: Neuroblastoma known as ganglioneuroma only comprises developed nerve cells and is often not malignant. Ganglioneuromas are frequently found by chance during imaging examinations performed for other reasons and do not need to be treated.
- Mixed tumors:Neuroblastoma and other malignant or non-cancerous cell types can coexist known as mixed tumors. The kind and quantity of the various cell types present determine the prognosis for mixed malignancies.
Examining tumor cells under a microscope reveals the histology of the tumor. In addition to histology, additional elements including the child's age, the tumor size, and location, and whether it has spread to other body areas affect neuroblastoma treatment choices and prognosis.
Shedding light on innovative diagnostic tools for detecting neuroblastoma
Imaging studies, clinical testing, and laboratory tests are frequently combined in the diagnostic process for neuroblastoma. These tests can assist medical professionals in confirming the diagnosis, determining cancer's extent, and creating a suitable treatment strategy.
Imaging exams:
- Ultrasound: An ultrasound is a device that produces pictures of the body using high-frequency sound waves. This examination can assist in identifying a lump or tumor in the abdomen, which is where neuroblastomas are most frequently seen.
- Computed tomography (CT) scan: A CT scan uses computer technology and X-rays to create detailed images of the body. This examination can offer more thorough details on the size and location of a tumor as well as if it has been distributed to other regions of the body.
- Magnetic resonance imaging (MRI): A powerful magnetic field and radio waves are used in an MRI to provide detailed images of the body. This examination can offer thorough details on the extent, size, and placement of a tumor.
- Metaiodobenzylguanidine (MIBG) scan: Using a radioactive tracer, the metaiodobenzylguanidine (MIBG) scan is a specific form of nuclear medicine imaging that shows the body's regions where neuroblastoma cells are present. Finding tiny tumors or locations where the disease has spread can be made much easier with the use of this test.
Clinical evaluations
- Physical examination: A medical professional will often do a physical examination to check for indications of neuroblastoma, such as a bulge in the belly, bone discomfort, or unexplained weight loss.
- Biopsy: A biopsy is taking a little sample of tumor tissue and studying it under a microscope. This test can assist assess cancer's stage and grade as well as confirm the diagnosis of neuroblastoma.
- Biopsy of the bone marrow: A small sample of bone marrow is removed from the hip bone during a bone marrow biopsy and viewed under a microscope.
Lab examinations
- Blood testing: Blood tests can be used to identify particular compounds generated by neuroblastoma cells, such as catecholamines or enolase, that are unique to neurons (NSE).
- Urine Testing: Screens for chemicals in the urine that neuroblastoma cells generate, such as catecholamines or vanillylmandelic acid (VMA).
- Genetic Testing: Tests for particular genetic mutations or chromosomal abnormalities that may be connected to neuroblastoma can be found through genetic analysis.
Generally, to diagnose and stage neuroblastoma, a combination of these imaging techniques, clinical testing, and laboratory investigations is frequently employed. This data is essential for selecting the best course of treatment for each patient.
Leading your way to neuroblastoma treatment and care
Age, illness stage, and the genetic makeup of the tumor are only a few of the variables that affect neuroblastoma treatment.
Common neuroblastoma therapies include surgery, chemotherapy, radiation therapy, immunotherapy, and targeted therapy. Depending on the disease's stage and severity, several treatment strategies are used.
- Surgery: To stop cancer from spreading, surgery is conducted to remove the tumor and any nearby lymph nodes. Depending on where the tumor is, the surgeon may need to remove further nearby organs. Surgery might not always be an option, depending on the tumor's size and location.
- Chemotherapy: In the majority of cases with neuroblastoma, chemotherapy is administered either before or after surgery or, in rare situations, as the only form of treatment. Chemotherapy includes administering medications that either kill or inhibit the growth of cancer cells. Chemotherapy medications are often administered intravenously or orally, and the procedure is typically carried out in cycles with breaks in between. Depending on the disease's stage and severity, the type of chemotherapy and the number of rounds will vary. The chemotherapy medicines cyclophosphamide, vincristine, doxorubicin, cisplatin, and etoposide are used to treat neuroblastoma.
- Immunotherapy: A more recent form of treatment called immunotherapy makes use of the immune system to combat cancer. Targeting particular proteins on the surface of cancer cells with immunotherapy medications, such as monoclonal antibodies or checkpoint inhibitors, enables the immune system to recognize and destroy the cancer cells. Dinutuximab is an immunotherapy medicine used to treat neuroblastoma that specifically targets the GD2 protein that is present on the surface of neuroblastoma cells.
- Radiotherapy: In certain cases, radiation therapy is performed in combination with surgery and chemotherapy, especially when the tumor is big or has spread to lymph nodes or adjacent tissues. High-energy X-rays or other forms of radiation are used in radiation treatment to destroy cancer cells. Generally, radiation therapy is dispensed daily over several weeks. Isotretinoin, a retinoid that can aid in tumor reduction, is one of the radiation therapy medications used to treat neuroblastoma.
- Targeted therapy: Targeted therapy medications are used to specifically target particular genetic abnormalities or other molecular alterations in cancer cells. When a tumor carries a specific genetic mutation, such as MYCN amplification, targeted treatment is frequently performed. Targeted therapy medications are often administered orally, intravenously, and in cycles. Drugs used in targeted therapy for the treatment of neuroblastoma include crizotinib, which works against the genetic mutation ALK that has been identified in some instances of the disease.
In conclusion, depending on the stage and severity of the disease, neuroblastoma is treated with a mix of surgery, chemotherapy, radiation therapy, immunotherapy, and targeted therapy. A multidisciplinary team of medical experts, including surgeons, oncologists, radiologists, and pediatricians, may be involved in the treatment plan, which is frequently customized to the needs of each patient.
Every child deserves a chance: raise awareness against neuroblastoma and inspire action.









