A form of protein in red blood cells called methemoglobin carries oxygen in the body. When there is a particular gain in the amount of this component in blood, there occurs a medical condition which is called...
The First Step for Conquering a Disease Is Knowing About It - Introduction.
A form of protein in red blood cells called methemoglobin carries oxygen in the body.
When there is a particular gain in the amount of this component in blood, there occurs a medical condition which is called Methemoglobinemia.
Normally, only a small percentage of hemoglobin is in the form of methemoglobin, but in methemoglobinemia, the number of methemoglobin increases, making it difficult for the body to transport oxygen to the tissues. This can further cause problems such as shortness of breath, fatigue, and bluish discoloration of the skin.
The More We Know About This Disease, The Better Equipped We Are to Fight It - Epidemiology.
Inherited forms of methemoglobinemia are relatively uncommon and occur in less than 1 in 100,000 people. The most common form of inherited methemoglobinemia is due to a deficiency in the enzyme NADH-methemoglobin reductase, which is also known as cytochrome b5 reductase. This form of the condition is more common in certain populations, such as people of Native American and Middle Eastern descent.
Acquired methemoglobinemia is also relatively rare, but its incidence can be higher in certain populations or under certain circumstances. For example, exposure to certain drugs, chemicals, or toxins can increase the risk of developing methemoglobinemia. Nitrite-induced methemoglobinemia is more common in infants who have been given contaminated water, whereas chemical-induced methemoglobinemia may be more common in industrial workers who have been exposed to certain chemicals.
Overall, the incidence of methemoglobinemia is relatively low, and the condition is more likely to occur in certain populations or under certain circumstances. Early recognition and treatment are important to prevent serious complications and reduce the risk of long-term effects.
Unlocking The Mystery of Disease’s Pathogenesis.
Methemoglobinemia is a condition in which there is an uncommon gain in the amount of methemoglobin in the blood. Methemoglobin is a form of hemoglobin that is unable to carry oxygen effectively, and as a result, the tissues of the body may become oxygendeprived.
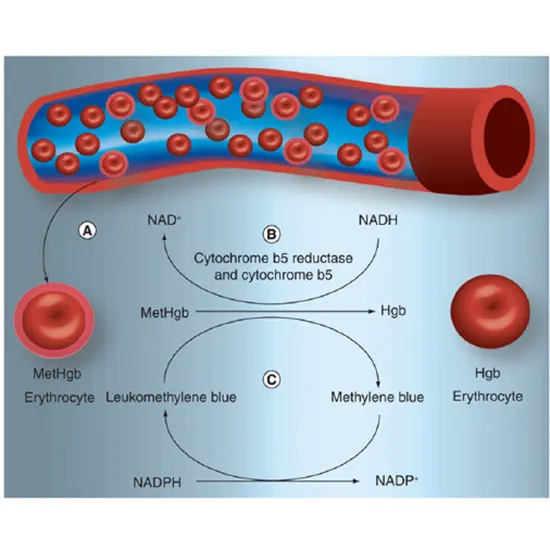
The normal hemoglobin molecule contains iron in its heme group, which can exist in either the ferrous (Fe2+) or ferric (Fe3+) state. Methemoglobin is a component that is formed when the heme group carrying iron is oxidized from the ferrous state to the ferric state, which makes it unable to bind to oxygen.
Methemoglobinemia can be inherited or acquired. Inherited forms of the condition resulting from mutations in genes that affect the production or function of enzymes that convert methemoglobin back to normal hemoglobin. For example, there are various types of genetic methemoglobinemia, including NADH-dependent methemoglobin reductase deficiency, cytochrome b5 deficiency, and hemoglobin M disease.
Acquired forms of methemoglobinemia can result from exposure to certain medications, chemicals, or toxins that can cause the conversion of normal hemoglobin to methemoglobin. Examples of these include certain antibiotics, nitrites and nitrates (used in food preservation), aniline dyes, and certain industrial chemicals such as benzene and chloroform.
In summary, methemoglobinemia results from an imbalance between the formation of methemoglobin and the body's ability to convert it back to normal hemoglobin. This leads to reduced oxygen transport and can result in tissue hypoxia, which can cause a variety of symptoms.
Various Types of Methemoglobinemia.
There are two main types of methemoglobinemia: inherited and acquired.
1. Inherited Methemoglobinemia: This type of methemoglobinemia is caused when there are mutations in genes that affect the production or function of enzymes that convert methemoglobin back to normal hemoglobin. There are several types of inherited methemoglobinemia, including:
- NADH-dependent methemoglobin reductase deficiency: This is the most common form of inherited methemoglobinemia. It is caused by a deficiency in the enzyme.
- NADH-methemoglobin reductase, which is necessary to convert methemoglobin back to normal hemoglobin.
- Cytochrome b5 deficiency: This type of methemoglobinemia is caused by a deficiency in the enzyme cytochrome b5, which is necessary to produce the enzyme NADH-methemoglobin reductase.
- Hemoglobin M disease: This is a rare genetic disorder that affects the structure of hemoglobin and results in the production of abnormal hemoglobin that is more prone to oxidation.
2. Acquired Methemoglobinemia: This type of methemoglobinemia is caused by exposure to certain medications, chemicals, or toxins that can cause the conversion of normal hemoglobin to methemoglobin. Some common causes of acquired methemoglobinemia include:
- Nitrite-induced methemoglobinemia: This can occur after ingestion of contaminated water or food that contains high levels of nitrates or nitrites.
- Chemical-induced methemoglobinemia: This can occur after exposure to certain chemicals, such as benzocaine, dapsone, or aniline dyes.
- Medication-induced methemoglobinemia: This can occur after exposure to certain medications, such as benzocaine, dapsone, or certain antibiotics, including nitrofurantoin and sulfonamides.
- Anesthesia-induced methemoglobinemia: This can occur as a rare side effect of anesthesia, particularly with the use of certain medications, such as prilocaine.
Let's Know the Culprits Of This Condition.
Methemoglobinemia is caused by an increase in the amount of methemoglobin in the blood. Methemoglobinemia can be caused by inherited genetic mutations or acquired through exposure to certain substances or medical conditions.
- Inherited methemoglobinemia: Inherited methemoglobinemia is caused when there are mutations in genes that influence the exhibition or function of enzymes that convert methemoglobin back to normal hemoglobin. There are several types of inherited methemoglobinemia, including NADH-dependent methemoglobin reductase deficiency, cytochrome b5 deficiency, and hemoglobin M disease.
- Acquired methemoglobinemia: Acquired methemoglobinemia is caused by exposure to certain medications, chemicals, or toxins that can cause the conversion of normal hemoglobin to methemoglobin
It is important to note that methemoglobinemia can also occur as a result of certain medical conditions, such as glucose-6-phosphate dehydrogenase (G6PD) deficiency, or as a complication of certain medical procedures, such as bronchoscopy.
Taking action against this condition starts with recognizing the symptoms.
In some cases, methemoglobinemia may cause no symptoms at all, while in other cases, it can lead to life-threatening complications. Common signs and symptoms of methemoglobinemia include:
- Cyanosis: One of the most characteristic symptoms of methemoglobinemia is cyanosis, a bluish discoloration of the skin and mucous membranes. Cyanosis may be present in the lips, tongue, nail beds, and around the eyes.
- Shortness of breath: Methemoglobinemia can cause shortness of breath and difficulty breathing, particularly during physical activity or exertion.
- Fatigue: Methemoglobinemia can cause fatigue and weakness, which may be exacerbated by low oxygen levels in the blood.
- Headache: Methemoglobinemia can cause headaches and dizziness, which may be a result of reduced oxygen supply to the brain.
- Confusion and disorientation: In severe cases, methemoglobinemia can cause confusion, disorientation, and loss of consciousness.
- Chest pain: Methemoglobinemia can cause chest pain, which may be a result of reduced oxygen supply to the heart muscle.
- Seizures: In rare cases, methemoglobinemia can lead to seizures and other neurological symptoms.
It is important to note that the severity of methemoglobinemia symptoms may not always correspond with the level of methemoglobin in the blood. In some cases, even low levels of methemoglobin can cause severe symptoms, while in other cases, high levels may cause no symptoms at all. It is important to seek medical attention if you experience any unusual symptoms or if you have been exposed to a substance that can cause methemoglobinemia.
Be Aware of Blue: Certain Factors Can Turn Your Blood Toxic - Risk Factors.
The risk factors of methemoglobinemia can include:
- Medications and chemicals: Certain medications and chemicals can cause methemoglobinemia. These can include topical anesthetics such as benzocaine, prilocaine, and lidocaine, as well as nitrites and nitrates found in fertilizers, water, and certain processed foods.
- Genetic factors: Methemoglobinemia can be inherited as an autosomal recessive trait, which means that both parents must carry a replica of the mutated gene for their child to be at risk of the condition.
- Exposure to nitrate-containing substances: Nitrates are commonly found in fertilizers, water, and certain processed foods. Disclosure of these implications can boost the danger of methemoglobinemia, especially in infants who may not have fully developed methemoglobin reductase enzyme.
- Occupational exposure: Certain occupations may put individuals at risk of methemoglobinemia, such as those working in the agriculture or chemical industry where exposure to nitrates and nitrites is more common.
- Infants under six months: Infants under six months of age are at an increased risk of methemoglobinemia due to their low levels of methemoglobin reductase enzyme, which helps to convert methemoglobin back to hemoglobin.
Don't Wait to Get Diagnosed Today - Diagnosis.
The diagnosis of methemoglobinemia typically involves a combination of medical history, physical examination, and laboratory tests.
- Medical history: The doctor will ask about the patient's symptoms, medical history, medications, and any exposure to chemicals or substances that can cause methemoglobinemia.
- Physical examination: The doctor will perform a physical examination to check for signs of cyanosis which are referred to as bluish bruising of the derma and mucous membranes and other signs of methemoglobinemia.
- Laboratory tests: The diagnosis of methemoglobinemia is confirmed by laboratory tests, which measure the level of methemoglobin in the blood. This is typically done using a co-oximeter, which is a specialized instrument that can measure the level of various forms of hemoglobin in the blood.
In addition to measuring the level of methemoglobin, the doctor may also conduct other laboratory examinations to rule out other conditions that can cause similar symptoms, such as carbon monoxide poisoning or anemia.
Genetic testing may be accomplished to identify any inherited genetic mutations that can increase the risk of methemoglobinemia.
Compassionate Care for a Faster Recovery - Treatment.
The treatment for methemoglobinemia may depend on the harshness of the situation and the underlying reason.
Mild cases of methemoglobinemia may not require any treatment, as the body can convert methemoglobin back to normal hemoglobin over time. In cases where symptoms are present, treatment may include:
- Oxygen therapy: High levels of oxygen can help to convert methemoglobin back to normal hemoglobin when the methemoglobin level is less than 30%.
- Methylene blue: Methylene blue is a medication that can be used to convert methemoglobin back to normal hemoglobin. It is typically administered intravenously and is effective in treating methemoglobinemia caused by medications and chemicals.
- Blood transfusion: In severe cases of methemoglobinemia, a blood transfusion may be necessary to replace the methemoglobin with healthy red blood cells.
It is crucial to determine and deal with the underlying reason for methemoglobinemia, such as discontinuing medications or avoiding exposure to substances that can cause the condition. In cases of inherited methemoglobinemia, genetic counseling may be recommended to identify any future risks and prevent transmission to offspring.
Overall, prompt treatment is essential in cases of methemoglobinemia to preclude difficulties and provide a prosperous outcome.
Small Steps, Big Rewards: Invest in Disease Prevention.
Here are some tips for preventing methemoglobinemia:
- Avoid medications and chemicals that can cause methemoglobinemia: If you have a history of methemoglobinemia or are at risk for the condition, it is important to avoid medications and chemicals that can cause methemoglobinemia, such as benzocaine, prilocaine, and nitrites.
- Use caution when using topical anesthetics: If you need to use a topical anesthetic for medical or dental procedures, talk to your healthcare provider about using a low-dose or alternative medication that is less likely to cause methemoglobinemia.
- Check the nitrate levels in drinking water: If you rely on well water or other sources of drinking water, it is important to have the water tested for nitrate levels. If the grades are elevated, evaluate using a water therapy system to reduce the nitrate levels.
- Be cautious with processed foods: Some processed foods, such as cured meats and hot dogs, contain nitrates that can increase the risk of methemoglobinemia. Limit your intake of these foods or look for nitrate-free options.
- Use protective equipment: If you work in an industry where exposure to nitrates and nitrites is common, be sure to use defensive gear such as gloves and masks to minimize exposure.
- Genetic counseling: If you have a family history of methemoglobinemia, consider genetic counseling to assess the risk of transmitting the condition to offspring.
What If Left Untreated?
Complications may include:
- Hypoxia: Methemoglobinemia can reduce the amount of oxygen that is transported to the body's tissues, leading to hypoxia (low oxygen levels in the blood).
- Seizures: In severe cases of methemoglobinemia, seizures may occur due to an absence of oxygen to the brain.
- Organ damage: If methemoglobinemia is not treated promptly, it can lead to damage to the heart, lungs, liver, and other organs due to hypoxia.
- Death: In rare cases, severe methemoglobinemia can be life-threatening, especially when not analyzed and dealt with promptly.









