Jaundice, also referred to as hyperbilirubinemia, is characterised as a yellow discolouration of bodily tissue brought on by the buildup of too much bilirubin. Bilirubin deposition only occurs when there is an excess of...
What is Jaundice?
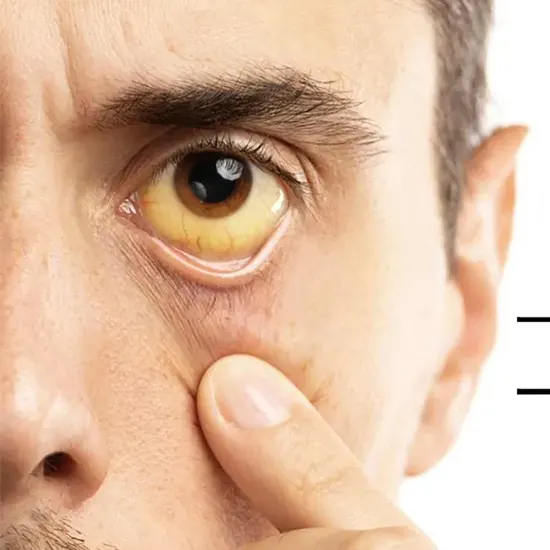
Jaundice, also referred to as hyperbilirubinemia, is characterised as a yellow discolouration of bodily tissue brought on by the buildup of too much bilirubin. Bilirubin deposition only occurs when there is an excess of bilirubin, which suggests increased production or impaired excretion.
Less than 1 mg/dL of bilirubin is considered to be the normal amount in serum. However, when serum bilirubin levels surpass 3 mg/dl, it is easiest to understand the clinical presentation of jaundice with peripheral yellowing of the eye sclera, also known as scleral icterus. The skin will gradually turn from lemon yellow to apple green as serum bilirubin levels rise, particularly if the process is ongoing. The green hue is caused by biliverdin.
Jaundice can be caused by either of bilirubin's two components—unconjugated (indirect) or conjugated (direct)—elevating. In addition to other insults, icterus serves as a crucial clinical indicator for liver illness. Carotenoderma is characterised by yellowing of the skin that spares the sclerae and affects healthy people who eat an excessive amount of foods high in carotene.
Etiology Behind Jaundice
Hyperbilirubinemia Conjugated:
- Defect in organic anion transfer in the canaliculus
- Dublin Johnson disease
- Sinusoidal absorption of conjugated bilirubin is defective.
- Condition rotor
- Reduced elimination of bilirubin from the liver
- The hepatocellular disease includes cirrhosis, nonalcoholic steatohepatitis, EBV, CMV, HSV, Wilson, autoimmune, and viral hepatitis A, B, and D.
- Primary biliary cholangitis and primary scelrising cholangitis are symptoms of cholestatic liver illness.
- Invasive illnesses (e.g., amyloidosis, lymphoma, sarcoidosis, tuberculosis)
- conditions of sepsis and hypo-perfusion
- complete intravenous alimentation
- Oral contraceptives, rifampin, probenecid, steroids, chlorpromazine, herbal medicines (such as Jamaican bush tea, kava), and arsenic are among the drugs and toxins.
- in sickle cell illness, hepatic crisis
- Pregnancy
Extra-Hepatic Choleostasis (Biliary Obstruction)
- Choledocholithiasis
- Tumors (e.g., cholangiocarcinoma, head of pancreas cancer)
- Additional biliary atresia
- Chronic and acute pancreatitis
- Parasitic diseases (e.g., Ascaris lumbricoides, liver flukes)
Unconjugated Hyperbilirubinemia
- Excessive bilirubin generation
- Extravasation of blood into organs, dyserythropoiesis, and haemolytic anaemia
- Reduced bilirubin hepatic absorption
- Syndrome Gilbert
- Conjugation issues
- Types 1 and 2 of Crigler-Najjar syndrome
- Hyperthyroid
- Oestrogen
Epidemiology Related to Jaundice
In different patient groups, jaundice is more common; it is more prevalent in newborns and the elderly.
As was already stated, there are various age-related causes of jaundice. Jaundice affects about 20% of term babies in their first week of life, mostly because of an immature hepatic conjugation mechanism. Jaundice that manifests in infancy or youth can also be brought on by congenital disorders, excess hemolysis production, poor bilirubin uptake, and poor conjugation. The most common source of jaundice in children was discovered to be hepatitis A. In the geriatric population, bile duct stones, drug-induced liver disease, and malignant biliary obstruction are common.
Men are more likely to develop cirrhosis, both drunken and nonalcoholic, chronic hepatitis B, pancreatic cancer, or sclerosing cholangitis.
The prevalence of gallbladder cancer, primary biliary cirrhosis, and gallbladder stones are greater in women.
Kernicterus, also known as bilirubin-induced neurologic dysfunction (BIND), is a very uncommon cause of neonatal death with a mortality incidence of 0.28 per one million live births. It is a complication of severe jaundice.
Pathophysiology of Jaundice
The pre-hepatic, hepatic, and post-hepatic phases of bilirubin metabolism provide the finest framework for understanding the pathophysiology of jaundice.
Pre-Hepatic
Heme, which is produced by aged or damaged RBCs, eventually gives rise to bilirubin. Heme released from the RBC experiences a series of reactions in the reticuloendothelial cells of the spleen, liver, and bone marrow to produce the final product.
bilirubin:
Heme-->Biliverdin-->Bilirubin (insoluble due to tight hydrogen bonding)
Hepatic
- Hepatocellular uptake: The non-soluble, unconjugated form of bilirubin produced by the reticuloendothelial system is transported to the hepatocytes where it is bound to albumin to achieve solubility in the blood. The bilirubin-albumin binding is shattered, and the bilirubin is then transported into the hepatocytes via carrier-membrane transport and bound to proteins in the cytosol to lessen bilirubin efflux back into the plasma.
- Following its journey to the endoplasmic reticulum, this unconjugated bilirubin endures conjugation to glucuronic acid, creating conjugated bilirubin, which is soluble in bile. UDP-glucuronosyl transferase is responsible for producing this.
Post-Hepatic
- Conjugated bilirubin is now discharged from the hepatocytes and travels through the bile ducts, gallbladder, ampulla of Vater , small intestine, and colon before ending up in the colon.
- Conjugated bilirubin's hydrophilicity and big molecular size prevent the intestinal mucosa from reabsorbing it. The enterohepatic circulation of the remaining 10 to 20% occurs as a result of the colonic bacteria's deconjugation and metabolism of bilirubin into urobilinogens, of which 80% are expelled in the faeces and stercobilin. The kidneys excrete some of these urobilins, which gives urine its characteristic golden colour.
Unconjugated bilirubin levels in the serum rise due to dysfunction in the pre-hepatic phase, whereas increased conjugated bilirubin levels are caused by injury in the post-hepatic phase. Unconjugated and conjugated bilirubin levels can both increase due to hepatic phase dysfunction.
Increased bilirubin synthesis, increased re-absorption of urobilinogen from the colon, or reduced hepatic clearance of urobilinogen can all lead to increased urinary excretion of the substance.
Histopathology Of Jaundice
The four distinct types of intrahepatic cholestasis are as follows:
- Fine yellow pigment (bile) fills the cytoplasm of liver cells in cytoplasmic cholestasis.
- Bile is discovered in the canaliculi in canalicular cholestasis.
- Bile buildup in the Hering periportal bile ductules is referred to as ductular cholestasis. Ductular cholestasis is linked to sepsis and serious obstruction.
- Bile casts can be seen in the portal bile channels due to a condition called ductal cholestasis.
The detergent impact of retained bile acids appears to be the cause of the histopathological changes caused by excess bile.
Symptoms
- Apart from a yellowish discolouration of the skin and pruritus, patients typically appear with a variety of symptoms, which help to narrow down the aetiology or they may be asymptomatic. The use of drugs, alcohol, or other toxic substances, hepatitis risk factors (travel, risky sexual behaviour), HIV status, personal or family history of any inherited disorders, or haemolytic disorders must all be thoroughly questioned. The length of jaundice and the existence of any additional symptoms, such as joint pain, a rash, myalgia, and changes in urine and stool, are also crucial considerations.] Hepatitis caused by drugs or viral illnesses is indicated by a history of arthralgia and myalgias prior to the onset of yellowing.
- Further, fever, chills, severe right-upper-quadrant-abdominal pain as seen in cholangitis and anorexia, malaise as seen in hepatitis and significant weight loss suggesting malignancy obstructing the bile ducts provide additional information for diagnosis. Additionally, a patient with a history of ulcerative colitis may present with hyperbilirubinemia due to PSC.
Physical Examination in Case of Jaundice
The evaluation of body habits and the nutritional state starts a physical examination. Muscle wasting in the proximal and temporal limbs indicates cancer or cirrhosis.] It is important to go over the well-known stigmata of chronic liver disease, which include testicular atrophy, parotid gland growth, gynecomastia, caput medusae, spider nevi, and palmar erythema. Additionally, palpable lymph glands can alert a doctor to cancer. (left supraclavicular & periumbilical). Jugular venous distension, a symptom of increased volume status in the patient and an indication of hepatic congestion can indicate right-sided heart failure.
The abdominal inspection should reveal whether hepatosplenomegaly or ascites are present. Ascites and jaundice are signs of either cirrhosis or peritoneal dissemination of malignancy.
The Courvoisier sign, which is right upper quadrant pain with palpable gallbladder, denotes cystic duct obstruction brought on by cancer.
Diagnosis
- The most crucial laboratory test to perform is a liver function test after taking a comprehensive medical history and performing physical exams.
- Aspartate transaminase (AST), alanine transaminase (ALT), alkaline phosphatase (ALP), gamma-glutamyltransferase, serum albumin, protein, and bilirubin levels are measured during liver function exams.
- ALP levels should be low but AST, ALT, and liver transaminase levels should all rise if the injury is hepatic in origin.
- Alcoholic liver disease is characterised by an AST/ALT level greater than 2. When the AST and ALT readings are in the 1000s, toxins like acetaminophen, ischemia, or viruses are most likely to blame for the hepatocellular disease.
- The most probable cause is biliary obstruction if ALP levels are five times above normal and liver transaminases are normal or less than two times normal. By ordering a GGT serum profile, it is possible to distinguish between bone disorders and the elevated serum ALP levels associated with biliary injuries; higher levels indicate a hepatic origin.
- If the AST, ALT, and ALP values are normal, liver or bile duct damage is not the cause of the jaundice. Pre-hepatic conditions such as blood disorders, inherited liver conjugation disorders, or defects in hepatic excretion must be the reason. (Rotor, Dubin-Johnson).
- Unconjugated or conjugated bilirubin levels in the blood are rising. All jaundiced patients should undergo extra tests in addition to the liver panel, such as the albumin and prothrombin time tests, which are indicators of chronic and acute liver function, respectively. Prothrombin time's failure to decrease after receiving parenteral vitamin K indicates severe hepatocellular dysfunction.
- The outcomes of the bilirubin, enzyme, and liver function tests will point the doctor in the direction of a hepatocellular or cholestatic cause and provide some insight into the length and intensity of the illness.
- Based on the preliminary review, further analysis can be carried out.
- Viral serologies, inflammatory antibodies, serum ceruloplasmin, and ferritin are all part of the hepatocellular workup.
- Additional procedures for cholestatic workup include abdominal ultrasound, computed tomography (CT), magnetic resonance cholangiopancreatography (MRCP), and endoscopic retrograde cholangiopancreatography.
Treatment/Management
When feasible, the best way to treat jaundice is to treat the underlying hepatobiliary or haematological condition.
- Depending on the severity, cholestasis-related prorates can be controlled. Warm baths or oatmeal baths can be soothing for minor pruritus. Pruritus can also benefit from antihistamines.
- Bile acid sequestrants like cholestyramine or colestipol work well for patients with mild to severe pruritus.
- Rifampin, naltrexone, sertraline, or phenobarbital are some additional treatments that are less successful. If all other medical options are unsuccessful, liver surgery may be the only cure for pruritis.
- Depending on the severity of the hepatic injury, jaundice is a sign of hepatic decompensation and may warrant consideration for a liver transplant.
Differential Diagnosis
For skin discolouration that is yellowish, the difference is small. Carotenoderma, a condition that typically spares the sclerae, can manifest in healthy people who consume large amounts of carotene-rich vegetables and fruits, such as carrots.
Up to one-third of patients receiving quinacrine experience skin discolouration that is yellow in colour
Summary/Preventive Measures
Jaundice from resorption of hepatomas, newborn physiologic jaundice, breastfeeding, breast milk jaundice, Gilbert syndrome, and choledocholithiasis are among the aetiologies of the condition with good prognosis.
Malignant biliary obstructions and cirrhosis with jaundice typically indicate a worse outlook.
Most cases of jaundice can be effectively prevented by following a few simple recommendations which include:
- Avoid herbal medications without consulting with a physician, most herbal supplements are toxic to the liver and can cause irreversible liver damage leading to jaundice
- Avoid smoking, consumption of alcohol, and intravenous drugs
- Avoid exceeding the recommended dose on prescribed medications
- Visit your doctor if you notice yellowish discolouration of body tissue
- Encourage safe sex practices
- Always get the recommended vaccines before traveling to a foreign country









