The majority of gastrointestinal stromal tumours (GISTs) present asymptomatically, are rare neoplasms of the gastrointestinal tract, best detected by computed tomography (CT) scan, and most stain positive for CD117 (C-Kit),...
What is Gastrointestinal Stromal Tumour
The majority of gastrointestinal stromal tumours (GISTs) present asymptomatically are rare neoplasms of the gastrointestinal tract, best detected by computed tomography (CT) scan, and most stain positive for CD117 (C-Kit), CD34, and/or DOG-1. There have been numerous risk stratification classification systems that are based on tumour size, mitotic rate, location, and perforation.
Initially, it was thought that the mesenchymal cells of the gastrointestinal system (GIT) were the source of gastrointestinal stromal tumours (GISTs). In 1998, Kindblom and colleagues discovered that these tumours actually develop from Cajal's interstitial cells. These tumours exhibit CD117 antigen (C-Kit), which Harota and associates found to be a gain of function mutation that stimulates the development of these tumours. Although GISTs are rare tumours, the actual prevalence of GISTs is unknown because the majority of GISTs are found by accident. Surgical resection has always been the cornerstone of treatment for GISTs because conventional chemotherapy and radiation are ineffective against them. The treatment has undergone a significant shift as a result of the identification of mutations linked to these tumours.
Epidemiology
GISTs are uncommon, making up just 1% to 2% of gut tumours. Between January 2000 and December 2014, Soured and colleagues examined 29 studies involving 13,550 patients from 19 various nations who had GISTs). The male to female ratio was 1:1, and the typical age was 65 (the range was 10-100). Hong Kong, Shanghai, Taiwan, and Norway had the greatest incidence rates (19-20 per million per year), according to research. The Chinese province of Shanxi had the lowest frequency, at 4.3 per million per year.
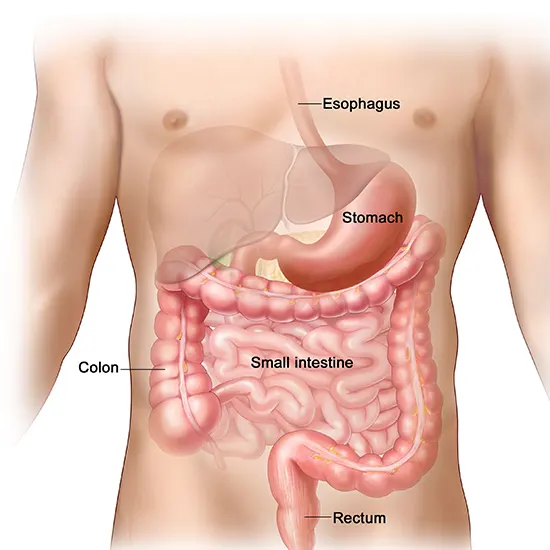
18% (interquartile range, 5–40%) of GISTs were stumbled upon. GISTs were discovered in the oesophagus (0.7%), colon and rectum (6%), small intestine (32%), stomach (56%), and other locations (5.5%). 10% to 30% of GISTs develop into cancer. GISTs that develop outside of the gut have a greater likelihood of developing cancer. In 79% of GISTs, exophytic growth is observed, whereas intraluminal or mixed development is less common.
Clinical Presentation
18% of instances of GISTs, particularly those involving smaller intestinal tract tumours, present without symptoms. These tumours are typically discovered by chance during endoscopies, surgery for other symptoms, or abdominal CT scans. Patients who are symptomatic may exhibit nonspecific symptoms such as abdominal discomfort, early satiety, abdominal distension, nausea, vomiting, and, in rare cases, a palpable abdominal mass. Depending on where the mass is, larger tumours may block the gastrointestinal lumen through endophytic growth or compress the GIT through exophytic growth, causing dysphagia, obstructive jaundice, or constipation.
There will be symptoms of peritonitis or gastrointestinal haemorrhage when a neoplasm has perforated. Pressure necrosis and ulceration are the secondary causes of mild to severe intraperitoneal haemorrhage.
Diagnostic Imaging
The most effective method for determining the position of these tumours, any perforation, invasion of these tumours into neighbouring structures, or metastasis is CT enterography .
GISTs can also be definitively diagnosed using CT-guided surgery. In instances of emergency or incidental tumour discovery, preoperative biopsy is not always necessary.
Abdominal ultrasound is helpful if the tumour is larger than 5 cm, even though it is not the main technique for visualising GISTs. However, a variety of variables, including the presence of necrosis, ulceration, the air in the bowel, and operator skill, have an impact on how reliable ultrasound is as a modality.
Ghanem and Colleagues divided the patients into groups based on tumour size and examined the results of CT imaging on patients with primary (n=20) or recurrent (n=16) GISTs. Using CT imaging, tumours were categorised as small (5 centimetre), intermediate (5–10 cm), or large (>10 cm).
By using CT imaging to visualise the tumours, Tateishi and coworkers investigated the histologic tumour grade and mortality rate in patients with low-grade (n=44) and high-grade (n=25) GISTs. They discovered that high-grade histology or higher mortality were both linked to tumours that measured more than 11.1 cm on a CT scan. These tumours were discovered to have irregular borders and margins, invasion of nearby tissues, and metastasis to the liver or peritoneum. They came to the conclusion that CT scanning can evaluate the tumour's size and metastasis, thereby predicting how well adjuvant treatments will work.
Although MRI is favoured when identifying rectal GISTs, liver metastasis, haemorrhage, and necrosis of tumours, it is comparable to CT imaging of GISTs in that it also provides information about size, tumour perforation, metastasis, and invasion into nearby structures.
While large GISTs look non-symmetrical and lobulated, small GISTs on MRI appear symmetrically round. However, CT has the benefit over MRI in that it shows the small bowel's entire thickness, making it easier to see the mesentery and deep ileal loops.
When combined with CT, 2-[F-18]-fluoro-2-deoxy-D-glucose PET scans offer helpful data for tumour staging. PET/CT imaging can be used to spot necrosis in lesions and tell innocuous tumours apart from malignant ones.
Invasive Imaging
In a retrospective analysis involving 174 patients who had GISTs surgically removed between 2008 and 2014, Park et al. investigated the use of endoscopy. While the remaining 65 (37.4%) exhibited extraluminal growth, it was found in 109 patients (62.4%); extraluminal growth was also seen in those cases. On endoscopy three months before detection, patients with intraluminal GISTs displayed smaller tumour sizes and ulceration while extraluminal GISTs went unnoticed. The researchers came to the conclusion that because extraluminal tumours are so common, endoscopy plays a relatively small part in the detection of GISTs.
Radio-Histopathologic Correletation
Histopathology and immunochemistry are used to diagnose GISTs. GISTs can exhibit spindle (70%), epithelioid (20%), or mixed type (10%) histologic results, among three other types. Prior to immunohistochemical analysis, they are frequently misidentified as leiomyoma or leiomyosarcoma. Microabscesses can also be seen on a microscope if tumours perforate. In about 88% of GISTs, CD117 and DOG-1 stain positively. A recent study of 70 GIST cases revealed that CD117 and DOG-1 were positively expressed in 95.71% and 88.57% of cases, respectively. According to the literature, DOG-1 is thought to be more sensitive and particular than CD117. However, their sensitivities drop to 9% and 79%, respectively, in GISTs with a PDGFRA mutant.
Risk Classification and Management
Over the years, many classification methods have developed, but none has emerged as the best. The first GIST classification scheme was developed by Fletcher and colleagues in 2002 and is known as the NIH classification. By examining the tumour's size and mitotic activity, it classified patients into very low, low, intermediate, and high-risk groups in order to identify their risk of recurrence. They came to the conclusion that tumours larger than 5 cm in diameter with a higher-than-5/50 high power field (HPF) mitotic count and tumours larger than 10 cm with any mitotic rate have a greater risk of recurrence, necessitating adjuvant drug therapy.
A new classification scheme known as the Armed Forces Institute of Pathology (AFIP) classification system was suggested by Miettinen and colleagues in 2006 after they evaluated 1,765 stomach GISTs and 906 small intestine GISTs. They found that anatomical position is a significant prognostic factor in addition to tumour size and mitotic rate. Additionally, they established the overall area for mitotic counting first. (5 mm2). According to this classification scheme, non-gastric GISTs have a higher recurrence risk than gastric GISTs for a tumour of the same size and mitotic count. The AFIP classification was updated by Goh and associates, who combined the very low and low risk into one category and added a very high-risk group.
Only tumours larger than 5 cm and having more than 10 mitoses per HPF had a high risk of recurrence, they discovered. There was no discernible difference in recurrence between the very low and low-risk categories. The modified NIH classification was developed in 2008 by Joensuu and colleagues, who found that tumour rupture during the operation had a gravely poor prognosis. If a GIST is >10 cm in size with any mitotic index, >5 cm in size with a mitotic count >5/50 HPF, or if the tumour has burst, the tumour is deemed high risk The most crucial prognostic factor for non-ruptured GISTs was found to be the mitotic rate, which also decides when adjuvant drug therapy is required.
Staging and Marking
The tumour-grade-metastasis (TGM) system was proposed by Woodall and colleagues as a means of determining a GIST staging scheme. They looked back at 2,537 GISTs that were diagnosed between 1977 and 2004. 48% of the patients were males, and the median age was 64. 23% of patients had spread and 5% had lymph node involvement at a follow-up of 21 months. Tumours classified as T1 under the TGM system are less than 70 mm in size, while tumours classed as T2 are larger than 70 mm. Grade I and II tumours are classified as G1 by the second criterion, and grade III and IV tumours as G2. Last but not least, metastasis was classified as M1 in existence and M0 in absence.
The most commonly used grading systems for soft tissue sarcomas are the National Cancer Institute (NCI) system and the French Federation of Cancer Centres Sarcoma Group (FNCLCC). Based on the tumour's division, necrosis, and mitotic activity, the FNCLCC grades the condition. This method shows a significant relationship between these variables and metastasis and mortality.)
The NCI method came to the conclusion that prognosis is determined by the quantification of cellularity, pleomorphism, and location. The effectiveness of imatinib as a neoadjuvant or adjuvant therapy can be assessed using the grading and staging methods for GISTs.
Surgical Treatment
The preferred way of treatment for unstable patients is an open laparotomy, even though laparoscopic surgery is the gold standard for treating GISTs. (33). For GISTs that are less than 5 cm and situated in the stomach and small intestine, laparoscopic surgery (LSG) is advised. Chen and colleagues examined 58 GIST instances in the past. LSG was used in 16 instances (27%) and open surgery was used in 42 cases (73%) (OSG). One LSG patient and two OSG patients both experienced recurrence after median follow-ups of 33 and 40 months, respectively. In comparison to the OSG group, the LSG group was able to restart a regular diet sooner, spent less time in the hospital after surgery, and needed less pain medication.
Adjuvant Treatment
The three medications imatinib (Gleevec), sunitinib (Sutent), and ponatinib are authorised for the treatment of GISTs. Imatinib is a TKI that inhibits signal transmission by attaching to the ATP-binding sites on CD117 and PDGFRA. PDGFRA and CD117-positive GISTs are believed to respond favourably to this treatment. DeMatteo and associates randomly assigned 713 patients with primary GISTs that were removed and measured more than 3 centimetres and stained for CD117. 359 individuals received imatinib and 354 received a placebo in randomisation. At one year, imatinib had a recurrence-free survival rate (RFS) of 98% compared to 83% in the control group (P 0.001). (8). Demetri and associates examined 147 individuals in 2002 who had metastatic or unresectable GISTs that expressed CD117. They were given either 400 mg or 600 milligrammes of imatinib per day at random.
Summary
Rare tumours called GISTs make up a tiny portion of gastrointestinal neoplasms. GISTs that develop outside of the stomach have a greater risk of developing into cancer. GISTs typically appear asymptomatically because they are often discovered incidentally. GISTs, on the other hand, can manifest symptomatically as nausea, vomiting, abdominal distension, abdominal discomfort, or peritonitis. GISTs can be seen on abdominal ultrasound, MRI, and PET scans, but a CT scan is the greatest tool for identifying them. GISTs have a disease made up of spindle cells, epithelioid cells, or a mixture of cell types. CD117 and DOG-1 most frequently stain positively in GISTs.
As research continues to grow in this area, newer studies are showing the effectiveness of novel therapies such as ipilimumab, nivolumab, and EUS alcohol ablation.









