In the uterus, fibroids, which are benign growths, develop. They can also be referred to as myomas, leiomyomas, or uterine fibroids. Muscle and fibrous tissue make up fibroids, which can range in size from small growths the...
What We Should Know About Uterine Fibroids?
What are fibroids?
- In the uterus, fibroids, which are benign growths, develop. They can also be referred to as myomas, leiomyomas, or uterine fibroids. Muscle and fibrous tissue make up fibroids, which can range in size from small growths the size of seeds to big ones the size of grapefruits.
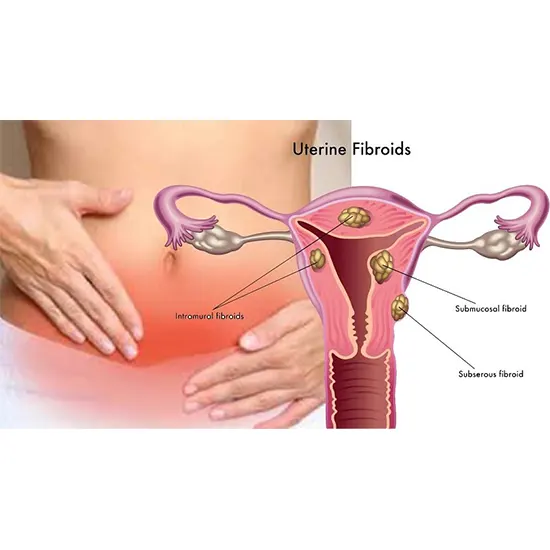
- Submucosal fibroids, subserosal fibroids, and uterine wall fibroids are some examples of the various areas of the uterus where fibroids can develop. (Intramural fibroids). Additionally, they can develop singly or in clusters.
- Those who have never given birth or who have a family history of fibroids are more likely to do so. Although fibroids typically do not cause cancer, they can still result in a variety of symptoms and problems that can impair a woman's quality of life.
Types of Fibroids:
Fibroids can take many different forms and grow in the cervix. The position of fibroids within the uterus determines how they are classified. There are three major categories of uterine fibroids:
- Submucosal fibroids: These tumours develop inside the uterus and, in some instances, can result in infertility as well as heavy or protracted menstrual bleeding. The least frequent form of fibroids are submucosal fibroids, but they can produce the most symptoms.
- Intramural fibroids: These fibroids grow within the wall of the uterus and can cause symptoms such as pelvic pain, heavy menstrual bleeding, and pressure on the bladder or rectum. Intramural fibroids are the most common type of fibroid.
- Subserosal fibroids: These fibroids grow on the outside of the uterus and can cause symptoms such as back pain, constipation, and a feeling of fullness in the abdomen. Subserosal fibroids are less common than intramural fibroids, but can still cause significant symptoms.
In rare instances, fibroids can form on the ligaments that support the uterus, on other organs in the pelvic region, or outside the uterus entirely. Some fibroids can be a combination of these kinds. Fibroids can differ in size and location, with some being small and others growing to be several inches in diameter.
Why does this occur?
Although there is no known reason for uterine fibroids, there are several factors that may play a role in their growth. These consist of:
- Hormones: Progesterone and oestrogen, two hormones that control the menstrual cycle, can encourage fibroids to develop. When hormone levels are strong during the reproductive years, fibroids tend to grow; when hormone levels are low after menopause, fibroids tend to shrink.
- Genetics: The emergence of uterine fibroids appears to have a hereditary basis. Women are more apt to develop fibroids themselves if their families have a history of having them.
- Age and Reproductive Status: Fibroids typically appear in women who are or who are planning to become pregnant, and they enlarge during pregnancy when hormone levels are elevated.
- Obesity: An elevated chance of developing fibroids has been linked to excess body weight, especially around the waist.
- African American women are more prone than women from other racial and ethnic groups to develop fibroids.
- Diet: Consuming a lot of red meat while consuming little in the way of fruits and vegetables may increase your chance of developing fibroids.
the signs of a uterine tumour:
- Numerous symptoms, including heavy or protracted menstrual flow, pelvic discomfort or pressure, issues with the bladder or bowels, backaches, and swelling or enlargement of the abdomen, can be brought on by them.
- Fibroids can occasionally result in infertility or repeated miscarriages. However, a lot of women with fibroids have absolutely no signs. Typically, a pelvic check, ultrasound, or MRI are used to make the diagnosis.
Risk elements:
Several risk factors, such as the following, can raise a woman's chance of developing uterine fibroids:
- Age: Although they can appear at any age, fibroids most frequently affect women in their 30s and 40s.
- Family history: Women who have fibroids in their family are more prone to get them.
- African American women are more likely to acquire fibroids than women of other races and ethnicities.
- Obesity: Women who are obese or overweight are more likely to acquire fibroids.
- Unbalanced hormones: Progesterone and oestrogen, the two hormones that regulate the menstrual period, can also promote the growth of fibroids. Fibroid development may be more likely in women with hormonal abnormalities, such as those with polycystic ovary syndrome (PCOS).
- Additionally, fibroids are less likely to develop in women who have had numerous pregnancies.
- Patients who have endometriosis and adenomyosis may be more prone to developing tumours.
- It's important to keep in mind that while having these risk factors may increase your likelihood of developing fibroids, many women can still develop them even if they don't. If you are worried about your chance for fibroids, talk to your healthcare provider.
Mother- Daughter Relationship in Uterine fibroids:
There is some data that suggests uterine fibroids may have a genetic component, which may influence mother-daughter relationships.
- According to studies, women are more likely to develop fibroids themselves if there is a family history of the condition, especially if their mother or sister has the condition. This indicates that some women may be predisposed to developing fibroids due to a genetic link.
- Additionally, uterine fibroids can affect a woman's quality of life and possibly strain relationships, including the mother-daughter bond, because they can result in a variety of symptoms, such as heavy menstrual bleeding, discomfort, and infertility.
- It's crucial to remember that not all women with a family history of fibroids will experience symptomatic development, and many women with fibroids are able to successfully manage their symptoms with a range of treatment options. The diagnosis and treatment of uterine fibroids can be made easier by mothers and daughters' open dialogue and support.
Role of Genetics:
Although the precise cause of fibroids is not yet completely understood, it is thought that genetics may contribute to the development of these tumours.
- According to research, some genetic abnormalities may contribute to the growth of fibroids. For instance, a sizable percentage of fibroid cases have been found to have mutations in the MED12 gene. The growth of fibroids has also been linked to the HMGA2, COL4A5, and COL4A6 genes.
- Additionally, it is well-known that women who have a family history of fibroids are more likely to acquire them. Studies have shown that women are two to three times more likely to develop fibroids themselves if they have a first-degree relative (such as a mother or sister) who has had them.
- It's essential to remember, though, that genetics are just one factor that could play a role in the development of fibroids. Age, ethnicity, obesity, and hormonal imbalances are some additional risk factors.
The finding needs to be done for uterine tumour:
- A visit to a healthcare professional is typically the first step in the diagnosis of uterine fibroids. The doctor will conduct a pelvic inspection to look for any uterine abnormalities.
The doctor may suggest additional tests if fibroids are identified to decide on the best course of therapy. Women who have fibroids occasionally may not show any signs and only need routine monitoring to make sure the fibroids are not expanding or posing any health risks.
Basic physical evaluation and medical history are frequently the first steps in the diagnosis of uterine fibroids, which is then followed by more sophisticated tests and imaging studies as necessary. The process of diagnosing uterine fibroids may entail the following steps:
- Physical examination: To check for any anomalies in the uterus or surrounding tissues, your doctor may conduct a pelvic inspection. This might entail feelings for lumps or growths with their fingertips.
- Medical history: Your doctor might inquire about your menstrual cycle, including the frequency and duration of your periods, as well as any signs you may be feeling, like pelvic discomfort, heavy bleeding, or trouble urinating.
- Imaging procedures: Imaging procedures can be used to visualise the uterus and detect the existence of fibroids, such as ultrasound, MRI, or CT scans. Your doctor may use these procedures to help them figure out how many, where, and how big the fibroids are.
- During a hysteroscopy procedure, a small, illuminated tube with a camera on the end is inserted into the uterus through the cervix to observe the interior of the uterus and check for any anomalies. This procedure might be used if your doctor thinks you have uterine tumours.
- In some cases, a microscopic examination of a small sample of uterine tissue to establish whether it is cancerous may be performed. If additional imaging test results are suspicious or if your doctor has cause to suspect the fibroids may be cancerous, this may be done.
- Blood tests: Your doctor may request blood tests in rare circumstances to look for hormone levels or other markers that may be linked to the emergence of fibroids.
- Ultrasound: This test produces images of the uterus by using sound waves, and these images can be used to determine the size, position, and quantity of fibroids.
- The MRI (magnetic resonance imaging) imaging test creates exact images of the uterus and tumours using a magnetic field and radio waves.
- Biopsy: A small tissue sample from the uterus may be taken in rare circumstances to rule out the chance of cancer.
- During a hysteroscopy procedure, a small, flexible tube with a camera is inserted through the cervix and vagina to observe the uterus' interior.
Precautionary measure every woman should in day-to-day life to prevent fibroids: -
There are several precautions that can aid in stopping the growth of uterine fibroids, such as:
- Keeping up a healthy diet: Consuming a diet high in fruits, veggies, and whole grains can aid in the prevention of uterine fibroids.
- Exercise frequently: Maintaining a healthy weight can help lower the chance of developing uterine fibroids.
- Manage your stress: Stress can harm your health in general and may be a factor in the growth of uterine fibroids. Learning stress-reduction methods like yoga or meditation can help.
- Limit your intake of booze and caffeine: Limiting your intake of these substances may help you avoid developing uterine fibroids.
- Oral contraceptives are one type of birth control that may help lower the chance of uterine fibroids developing.
- Visits to your doctor on a regular basis can help your doctor spot any possible health problems, such as uterine fibroids, before they become a problem.
- It's crucial to remember that while taking these precautions may help stop the growth of uterine fibroids, they are not an assurance.
Various treatment options:
The following summary of uterine fibroids treatments is organised from least effective to most effective:
- Patient observation: If the fibroids are small and not producing any symptoms, your doctor may advise patient observation over time rather than immediate treatment.
- Medications: Gonadotropin-releasing hormone (GnRH) agonists and birth control pills can both reduce the growth of fibroids and ease symptoms.
- Endometrial ablation: This minimally invasive treatment entails tearing apart the uterine lining to lessen menstrual bleeding brought on by fibroids.
- In this minimally invasive treatment, the fibroids are made to shrink and die by blocking the blood vessels that feed them with oxygen and nutrients. This is known as uterine fibroid embolization (UFE).
- Myomectomy: This surgical process removes the fibroids while protecting the uterus from damage, making it ideal for women who still want to become pregnant.
- Hysterectomy: To get rid of the uterus and the fibroids in extreme instances, a hysterectomy may be required.
- Ultrasound waves are used in the non-invasive magnetic resonance-guided focused ultrasound (MRgFUS) treatment to eliminate fibroids.
The suggested course of treatment for each patient will rely on several variables, including the size and location of the fibroids, the severity of the symptoms, the patient's age, medical history, and desire to preserve fertility. To decide on the best course of action for your particular situation, it's crucial to discuss the risks and advantages of each treatment option with your healthcare practitioner.
With symptoms like excessive menstrual bleeding, pelvic pressure, and pain, uterine fibroids can be a challenging and upsetting condition for many women. These symptoms can significantly lower their quality of life. Fortunately, there are several successful management and relief techniques for uterine fibroids symptoms. Depending on the patient's overall health and medical history, the size, location, and severity of the fibroids, as well as other factors. For the optimal course of action, women should discuss their symptoms with their doctor. With a range of treatment choices available, women with uterine fibroids can actively manage their condition and enhance their general health and wellbeing. Women can lessen the impact of fibroids on their everyday lives and regain control over their health by getting the right treatment.









