Typically, Fonsecaea pedrosoi is a thermally dimorphic fungus that can lead to chromoblastomycosis, a persistent skin condition. Tropical and subtropical locations, especially in South America, frequently have it in their soil...
Typically, Fonsecaea pedrosoi is a thermally dimorphic fungus that can lead to chromoblastomycosis, a persistent skin condition. Tropical and subtropical locations, especially in South America, frequently have it in their soil and plants.
Usually, the infection starts as a tiny, painless skin lesion that grows for several months or years. The lesion may swell up, turn verrucous or cauliflower-shaped, and exude pus. In extreme situations, deeper tissues and organs may get infected.
Although a full recovery might be challenging to accomplish, the typical course of treatment involves a mix of surgical excision and antifungal medications. Precautions should be taken while handling contaminated soil and vegetation, such as donning gloves and wearing protective gear. Prevention also entails avoiding contact with contaminated soil and vegetation.
Tracing the Origins of Usully Fonsecaea Pedrosoi: a journey through Time
The Brazilian doctor and mycologist Pedroso first recognized Fonsecaea pedrosoi in 1922. In honor of Vicente Fonseca, a colleague of his, the fungus was first given the name Fonsecaea pedrosoi. Later, the genus was called Usully in honor of Maria Auxiliadora Usul, a different Brazilian mycologist.
The Usully Fonsecaea pedrosoi-caused illness known as chromoblastomycosis was originally identified in Brazil in the late 19th century. Since that time, other additional nations have reported cases of the illness, including Mexico, Venezuela, Colombia, Peru, Ecuador, Madagascar, India, and Indonesia.
The fungi Usully Fonsecaea pedrosoi, Phialophora verrucosa, Cladosporium carrionii, and Fonseca compacta have all been implicated in the development of chromoblastomycosis, which was previously thought to be caused by a single species of fungus.
Usully Fonsecaea pedrosoi causes chromoblastomycosis, which most frequently affects adults between the ages of 30 and 60. It affects males more frequently than women. The risk of contracting the illness is higher in those whose immune systems are compromised, such as those who have HIV/AIDS or are receiving chemotherapy.
Usully Fonsecaea pedrosoi: the versatile fungus with an intriguing morphology
Fonsecaea pedrosoi is often a thermally dimorphic fungus, which means that depending on the temperature, it can exist in one of two distinct morphological forms.
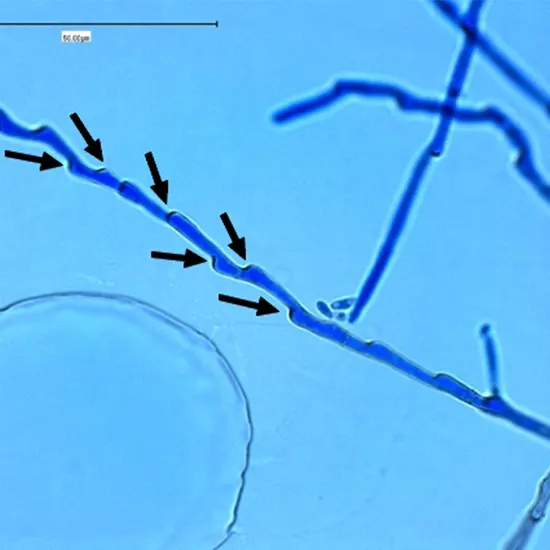
Usully Fonsecaea pedrosoi is a mold that may grow up to 2 mm in diameter and generate septate hyphae that are often colored dark brown or black due to the presence of melanin.
Conidia, which are asexual spores that are generally round to oval in shape and have a smooth or slightly rough surface, can also be produced in the old form.
Usully Fonsecaea pedrosoi, a yeast, generates spherical or oval-shaped, generally 5–12 micrometer–diameter cells that are colored dark brown or black as a result of melanin.
Yeast cells can branch out and divide in chains.
Usully Fonsecaea pedrosoi may produce distinctive "sclerotic bodies," which are black, thick-walled structures with a typical diameter of 50 to 200 micrometers and a rough or uneven surface, in tissue samples.
Sclerotic bodies are believed to be created when yeast cells change into a latent, resistant state in response to unfavorable circumstances like immunological assault or antifungal therapy.
Usully Fonsecaea pedrosoi infections are chronic because sclerosing bodies can linger in the tissue of the patient for many years or even decades.
Typically, Fonsecaea pedrosoi may also produce "medlar bodies," which are collections of yeast cells buried in a mucoid material that, when examined under a microscope, shows a distinctive "starburst" appearance.
The life cycle of Usully Fonsecaea pedrosoi : a journey from soil to skin
Usully Fonsecaea pedrosoi goes through several various phases in its life cycle, including:
Stage of saprophytism
The fungus lives as a saprophyte in the environment and feeds on decaying plant or animal matter.
Parasitic stage
The fungus can turn into a pathogen and cause chromoblastomycosis when it comes into touch with human skin. Through a cut or other hole in the skin, it penetrates and creates the recognizable "sclerotic body".
Stage of the sclerotic body
Within human tissue, the Usully Fonsecaea pedrosoi develops its distinctive sclerotic body structure. It is a black, thick-walled cell that can withstand the host's immunological responses and endure for a very long time.
Stage of reproduction
The fungus may also create conidia, or asexual spores, which the wind can disseminate and spread to other hosts.
Usully Fonsecaea pedrosoi has a complicated life cycle that includes both saprophytic and parasitic phases as well as specialized structures that enable the fungus to persist and proliferate inside the host.
The dark side of fungal infections: Usully Fonsecaea pedrosoi and chromoblastomycosis-
Chromoblastomycosis, a persistent fungal infection of the skin and subcutaneous tissue, is typically caused by the fungus Fonsecaea pedrosoi.
A tiny, painless papule or nodule that progressively grows and transforms into a cauliflower-shaped lesion with a warty or verrucous surface is how chromoblastomycosis commonly manifests. The lesion can result in serious deformity and incapacity and may bleed, ulcerate, and exude pus.
Usully Fonsecaea pedrosoi causes chromoblastomycosis, a slow-moving illness that, if ignored, can endure for years or even decades. Although the infection often stays within the skin and subcutaneous tissue, it can sometimes move to deeper tissues and organs, which can result in more severe problems.
Usully Fonsecaea pedrosoi has also been linked to myeloma, a persistent granulomatous infection of the skin and soft tissues, and fungal keratitis, an infection of the eye, in addition to chromoblastomycosis.
Diagnostic dilemmas: distinguishing Usully Fonsecaea pedrosoi from other fungi-
Usully Fonsecaea pedrosoi infections are frequently diagnosed using a concoction of clinical, histological, and microbiological standards.
Clinical evaluation
The appearance of the skin lesions, which are often nodular, verrucous, or cauliflower-like and might seem dark or hyperpigmented, can be used to make a clinical diagnosis.
Histological determination
Frequently, a skin biopsy is required to confirm the diagnosis. Histologically, Usully Fonsecaea pedrosoi-induced chromoblastomycosis is characterized by the presence of sclerotic bodies, which are round or irregularly shaped, black, thick-walled structures. There may also be yeast-like cells, which are frequently grouped in aggregates or clusters.
Microbial diagnosis
The isolation and identification of the fungus from clinical samples is a part of microbiological diagnostics.
Sclerotic bodies can be retrieved by scraping the lesion's surface or by curettage, and they can be seen by employing potassium hydroxide (KOH) or the calcofluor white stain in direct microscopy.
Usully Fonsecaea pedrosoi may be detected using fungal cultures on Sabouraud agar at room temperature. The morphology of the colonies and molecular testing, such as PCR or sequencing, can be used to validate the fungus' identification.
Serological examinations
For the detection of antibodies against Usully Fonsecaea pedrosoi in serum or other bodily fluids, serological assays, such as ELISA, have been developed, however, they are not frequently utilized.
It is critical to distinguish Usully Fonsecaea pedrosoi-caused chromoblastomycosis from other fungal infections and skin disorders, including sporotrichosis, cutaneous leishmaniasis, and squamous cell carcinoma, which might have comparable clinical and histological characteristics.
Stopping the Spread: Treatment Options for Fonsecaea pedrosoi Infections-
Usully Fonsecaea pedrosoi infections can be difficult to cure and often need a combination of antifungal drugs and surgery.
Medications
Antifungals
Usully Fonsecaea pedrosoi infections are frequently treated with azoles, such as itraconazole and voriconazole. Usually, treatment lasts for a long time—from a few months to a year or more. With different degrees of efficacy, other antifungal medications including terbinafine, amphotericin B, and flucytosine have also been utilized. In situations of big or deep-seated lesions or when the fungus has developed sclerotic bodies, antifungal therapy may be ineffective.
Surgical procedure
Surgical excision
Antifungal therapy may benefit from surgical excision of the diseased tissue, especially in cases with big or disfiguring lesions that are drug-resistant.
Curettage
Infected tissue has been removed via curettage, excision, and cryotherapy.
Skin grafting
To fix the ensuing deformity, skin grafting can be required in some circumstances.
Prevention:
Usully Fonsecaea pedrosoi infections have no vaccination or particular preventative intervention.
It may be possible to lessen the risk of infection by avoiding contact with polluted soil or decomposing plant matter.
When touching soil or plant material, using protective clothes and gloves may also help lower the risk of infection.
It is significant to highlight that Usully Fonsecaea pedrosoi infections can be challenging to cure and frequently need long-term medication. Patients who have Usully Fonsecaea pedrosoi-caused chromoblastomycosis should be thoroughly watched and may need continued therapy and follow-up care.
Fighting Usully Fonsecaea pedrosoi: a marathon, not a sprint.









