Splenic abscess is a rare but serious medical condition that occurs when pus-filled pockets develop in the spleen. The spleen is an organ located in the upper left side of the abdomen that plays a vital role in the immune...
Introduction:
Splenic abscess is a rare but serious medical condition that occurs when pus-filled pockets develop in the spleen. The spleen is an organ located in the upper left side of the abdomen that plays a vital role in the immune system and blood filtration. In most cases, the splenic abscess is caused by a bacterial infection, but it can also be caused by fungal or parasitic infections, as well as trauma or other medical conditions.
A splenic abscess can be a life-threatening condition if left untreated, as the infection can spread to other parts of the body and cause sepsis. This article will let you know about all the queries you have about Splenic Abscesses.
What is Splenic Abscess?
A splenic abscess is a medical condition characterized by the formation of a pus-filled cavity or collection of infected material within the spleen. The spleen is a vital organ located in the upper left abdomen that plays a key role in the immune system and blood filtration. Splenic abscesses are relatively rare and can occur as a complication of a bacterial infection, such as from the bloodstream or surrounding organs. Symptoms may include fever, abdominal pain, and an enlarged spleen, and treatment often involves antibiotics and drainage of the abscess. If left untreated, splenic abscesses can lead to serious complications, such as sepsis and rupture of the spleen.
What is the functioning of the Spleen?
To know about Splenic abscess, first, you should know about the spleen.
The spleen is a secondary lymphoid tissue that is located just above the stomach in the abdominal cavity. As such, it is a component of the lymphatic system. The spleen's main job is immunity; it also serves as a filter for pathogens that enter the bloodstream.
The spleen has various roles :
- It serves as a component of immune cell storage. These immune cells are transported by the spleen through circulation to the site of need.
- Additionally, it eliminates outdated, worn-out red blood cells.
- Additionally, it keeps platelets, which are in charge of clotting blood in the event of an accident.
The splenic artery and splenic vein supply the spleen, which is a highly vascularized tissue. Because the bone marrow, liver, and lymphoid organs also perform the tasks of the spleen, it is frequently regarded as a non-essential organ. Due to its location, the spleen is particularly vulnerable to damage and infection. If it is not addressed right away, a rupture of the organ could be fatal. Repair, partial splenectomy, and on rare occasions even complete splenectomy are among the available treatments.
How can you get encountered by splenic abscess?
Every disease has a process of pathogenesis. Let's learn about the various causes of splenic abscesses.
Due to the spleen's effective phagocytic activity, splenic abscesses are uncommon; however, in immunosuppressed patients (those with weakened immunity as a result of illnesses like cancer, diabetes, AIDS, etc.), the spleen's capacity to fight the infection is diminished, leading to infection and inflammation.
The major factors that cause splenic abscesses are:
1) Immunodeficiency Disorders
Cancer, chemotherapy, radiation treatment, AIDS, diabetes, transplant recipients, and autoimmune disorders are a few situations where the patient's immunity is weakened. Immune deficiency is brought on by the extended use of immunosuppressive medications, which put the spleen at risk for infections that lead to splenic abscesses in transplant recipients and people with autoimmune diseases.
2) Infection
While spleen-specific infection is rare, it can happen when an infection spreads from another organ (metastatic infection) or nearby contaminated tissue. (contiguous infection).
Infective endocarditis, endovascular infections, sepsis, lung abscess, diverticulitis, etc. are examples of metastatic infections.
Perinephric abscess and necrotic pancreatitis are two instances of concurrent illnesses.
Bacterial (Streptococcus, Staphylococcus), fungus (Mycobacterium), viral (HIV), or parasitic infections are possible. (Echinococcus granulosus). Patients getting embolisation therapy for a splenic artery pseudoaneurysm, which develops as a result of acute pancreatitis, occasionally developed a splenic abscess.
Splenic infarction is a situation in which the spleen's blood supply is impaired, leading to ischemia and necrosis. This raises the risk of a splenic abscess when combined with an illness.
3. Trauma:
The most frequent location of the injury, whether from an accident, blunt force trauma, or a fight, is the spleen. The spleen starts an inflammatory response to repair the damage, and this causes an abscess to develop.
Splenic abscesses are becoming more common among injectable drug users as well. Although a splenic abscess may not necessarily result in death, it is the primary cause of mortality in 80% of all affected patients when it occurs in conjunction with immunocompromised conditions.
Pathophysiology:
Splenic lesions are typically diagnosed as side effects of infective endocarditis, which affects 5% of patients. Streptococcus, Staphylococcus, (since endocarditis is the most frequent cause of splenic abscess), Mycobacterium, fungi, and parasites are frequently separated pathogens.
In some regions of the globe, Burkholderia pseudomallei can lead to splenic abscesses in susceptible people. The likelihood of dying is high and varies depending on immune function and the sort of abscess. Immunocompetent patients with unilocular abscesses have a fatality rate of 15%, while immunocompromised patients with multilocular abscesses have a mortality rate of up to 80%.
What Indicates a Splenic Abscess?
The most typical sign of splenic abscesses is fever, which patients experience. When the left upper quadrant of the belly is palpated, there may also be a tender mass there. In one-third of cases of splenic rupture, laboratory tests reveal leukocytosis (an increase in the number of white cells).
Various Features Seen in a patient suffering from splenic Abcess:
The signs of a splenic cyst are as follows:
- Fever. l
- In the upper left region, there is pain and tenderness.
- Leukocytosis (increased white blood cell count)
A physical evaluation will demonstrate:
- Guarding of muscles in the upper left region.
- Swelling in the nearby soft organs.
- Disc pain and stiffness.
- Right basilar rales.
- Dullness at the left lung's base.
Does Splenic Abscess Occur Frequently?
Splenic abscess is a rare disease that occurs between 0.05 and 0.7% of the time. Bacteremia is frequently to blame for it. To reduce mortality to under 10%, appropriate treatment with antibiotics is necessary.
Splenic abscess: Is it fatal?
According to reports, the fatality rate for splenic abscesses can reach 47%. The likelihood of this occurring can increase to 100% if the splenic abscess is left untreated or misidentified. Mortality can be lowered to under 10% with appropriate treatment using antibiotics, percutaneous drainage, or surgical splenectomy.
What Takes Place If the Splenic Abscess Isn't Drained?
A splenic abscess can develop into a deadly condition if it is not treated immediately. Pneumothorax, atelectasis, left-sided pleural fluid, pneumonia, life-threatening haemorrhage, subphrenic abscess, pancreatic fistula, perforation of the stomach, small intestine, or colon, and post-splenectomy thrombocytosis are some of the more serious side effects.
Which Tests Are Performed for a Splenic Abscess?
A splenic abscess can be identified using a variety of imaging techniques; the surgeon may order any of the following tests based on their availability:
- Plain radiograph
This is typically insensitive in assessing a splenic abscess, but it can aid in the initial diagnosis by using indirect indications.
On ultrasound, a splenic abscess is poorly defined and has gas bubbles and variable septal thickness. An ultrasound finding of hyperechogenicity and distal dirty shadowing indicates a splenic abscess.
Patients with the condition exhibit minimal peripheral enhancement, ascites, and nearby pleural fluid.
Depending on the abscess's extent and the infectious agent that is causing it, an MRI will have different imaging properties. An abscess with a proteinaceous substance, for instance, exhibits a low signal, while an abscess with a necrotic inflammatory infiltrate exhibits a high signal. (pus).
Nuclear medicine is a field of study in which radioactive substances are injected into the body to target diseased tissues. In the event of a splenic abscess, nuclear medicine may be used for both detection and treatment; scans using the radioactive forms of indium and gallium, indium 111 leukocyte and ga-67, respectively, will reveal the cavity of the abscess.
Treatment Options Available for Splenic Abscess:
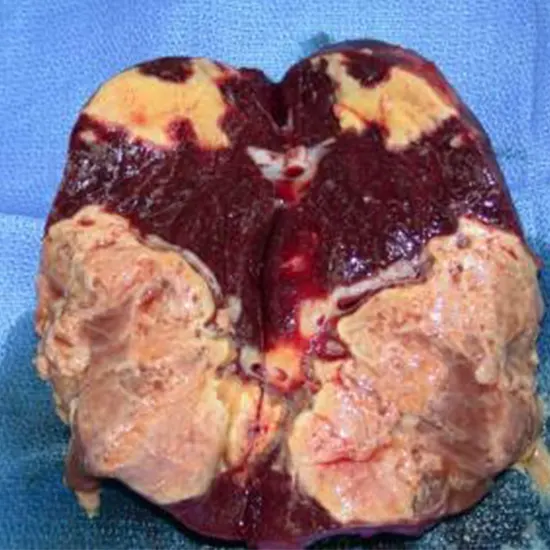
The gold standard for managing a splenic abscess is a splenectomy, which is the surgeon's last resort if high-dose parenteral broad-spectrum antibiotics are ineffective.
The operation may be performed in an open setting or with the aid of a laparoscope.
- Open splenectomy: Under anaesthesia, a midline incision is created in the belly that penetrates the skin.
- The muscles are drawn back, and the spleen's attached tendons are separated and tied. The related splenic artery and vein are anastomosed with a stapler after the spleen is mobilised by severing the adhesions. The spleen is meticulously removed from the body and removed in one piece before being sent for histopathological analysis.
Once hemostasis has been accomplished, the fascia is closed, and the edges of the skin overlying it are approximated and sutured. The physician then checks the area for any accessory spleens.
- Laparoscopic splenectomy - In this procedure, several small cuts are made rather than a single, significant one. One of the incisions is used to introduce a laparoscope, an instrument made of optic fibre with a camera attached to assist in visualising the underlying anatomy.
The operating room monitor receives real-time footage from the camera. After carefully inspecting the abdomen, the physician inserts specialised surgical tools through the accessory incisions and begins the spleen resection. A tiny incision is used to put the resected spleen into an endoscopic retrieval bag and remove it. The numerous incisions are stitched up once hemostasis has been achieved, and the patient is then moved to the intensive care section where they are watched until their vital signs are stable.
A minimally invasive procedure called percutaneous aspiration is another choice for treating splenic abscesses besides splenectomy. It is selected for patients who are at high risk for surgery and provides a temporary fix to prevent an infection that would otherwise be fatal.
What Are the Risks Associated with Percutaneous Aspiration and Splenectomy?
Spleen procedures carry the same risks of bleeding, infection, and haemorrhage as other types of operations.
Following splenectomy and percutaneous aspiration, particular complications include:
- Pneumothorax.
- Atelectasis.
- Potentially fatal haemorrhage.
- Pleural oedema on the left side
- A subphrenic cyst.
- Stomach, small intestine, and colon perforations.
- Fistula in the pancreas.
- Thrombocytosis following splenectomy.
- Pneumonia.
Splenectomy is always risky because patients are more vulnerable to infections after the procedure, so they should routinely refresh their immunisations.
In the past, a splenic abscess was thought to be an uncommon occurrence because it can be difficult to detect. However, with the development of new technology, clinicians can now quickly identify and treat splenic abscesses. Surgery and broad-spectrum antibiotics are combined to create an effective therapy plan. After the operation, the patient should be informed about the value of vaccinations and potential sepsis because the spleen, an effective immunomodulator, is no longer providing protection.
How long can you survive after having your spleen removed?
Even after having their spleen removed, a person can live a healthy and normal existence. An individual can still handle the majority of infections because other organs, like the liver, can compensate for the spleen's duties. However, a slight risk of infection could appear rapidly and last the rest of their lives.
How Serious Is a Spleen Cyst?
Because splenic cysts automatically burst, they must be regarded as high-risk lesions. Cystic rupture is a severe complication that is extremely rare but can result in peritonitis, abscess, hemoperitoneum, anaphylactic shock, and empyema.
Does a Splenic Abscess Require Surgical Attention?
Splenic abscess treatment usually involves physically removing the spleen. The diseased organ and the septic source are both removed during this operation. Specific individuals may benefit from the safe and successful procedure known as laparoscopic splenectomy.
Therefore, it is important to seek medical attention as soon as possible if you suspect you have a splenic abscess.
Prompt diagnosis and treatment are crucial for managing splenic abscesses and preventing potential complications.









