Polycythemia, or erythrocytosis, refers to an increase in the absolute red blood cell (RBC) mass in the body. In practice, this is reflected by an increase in haemoglobin levels, or hematocrits, over what...
What is Polycythemia?
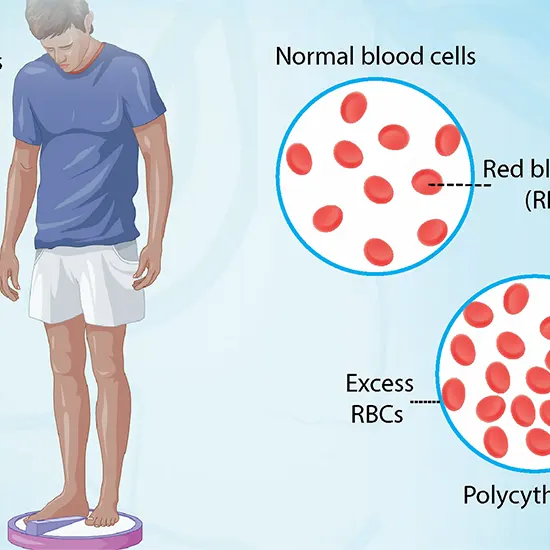
Polycythemia, or erythrocytosis, refers to an increase in the absolute red blood cell (RBC) mass in the body. In practice, this is reflected by an increase in haemoglobin levels, or hematocrits, over what is considered physiologic for the age and gender.
RBC quantity is typically no more than 32 ml/kg for women and 36 ml/kg for men. Depending on altitude, ethnicity, and nation, different reference values exist for normal haemoglobin levels and hematocrit. To put things in perspective, a robust adult male's haemoglobin and hematocrit are 16 g/dL +/- 2 gm/dl and 47% +/- 6%, respectively. A menstruating mature female typically has haemoglobin and hematocrit of 13 g/dL +/- 2 gm/dl and 40% +/- 6%, respectively. When a neonate has polycythemia, their central venous hematocrit is over 65% or their haemoglobin level is higher than 22 g/dL.
A subtype of polycythemia is polycythemia vera. It is an acquired, myeloproliferative disease with a Philadelphia-chromosome negative status that is frequently referred to simply as "polycythemia."
Any cause of erythrocytosis has clinical relevance because it increases the risk of thrombotic events because blood is more viscous. Additionally, the possibility of polycythemia vera cases progressing to leukaemia also justifies the implementation of additional treatment techniques.
Etiology:
Classification of polycythemia:
Artificial polycythemia
Rather than a rise in real RBC mass, this results from volume contraction.
A few factors are:
- Diarrhoea and severe vomiting can both lead to serious dehydration from isolated fluid loss.
- The Gaisbock condition Typically found in obese, hypertensive men.
- Diuretic use, excessive booze consumption, and smoking are all factors.
True Polycythemia
further classified according to blood erythropoietin (EPO) concentrations as follows:
- Low serum amounts of EPO (Primary polycythemia)
- A true polycythemia
- Hereditary and congenital primary polycythemia
Elevated blood EPO levels (Secondary polycythemia)
- High altitude
- Chronic obstructive pulmonary disease (COPD), Pickwickian syndrome, and uncontrolled asthma are examples of respiratory diseases.
- Right-to-left shunts in cyanotic cardiac conditions
- Renal diseases include focal sclerosing glomerulonephritis, focal sclerosing nephritis, renal cysts, renal artery stenosis, and kidney cancer.
- A higher level of carboxyhemoglobin People working on vehicles in enclosed spaces, particularly smokers.
Polycythemia in new-born
Infants' increased hematocrit is a typical defence strategy against the relative tissue hypoxia present in the intrauterine environment. The strong affinity of foetal haemoglobin for oxygen makes it worse.
Epidemiology
According to estimates from several sources, there are 22 instances of polycythemia vera per 100,000 people. Compared to other Europeans and Asians, Jewish patients of Eastern European descent are thought to experience it more commonly. Males predominate in polycythemia vera across all racial and cultural groups, with a male-to-female ratio of roughly two to one. PV patients are rarely seen before the age of 40, with a typical age of presentation of 60 years. Hemoglobinopathies and congenital cyanotic heart diseases are prone to cause polycythemia, and it is likely to be found in much younger patients.
Pathophysiology:
Depending on the cause under evaluation, the pathophysiology would change.
1. High Levels of EPO
Any factor that causes the renal peritubular lining capillary cells to produce erythropoietin can result in cellular hypoxia. The liver also produces a tiny amount of EPO. EPO also affects erythroid precursor cells, which in turn promotes erythropoiesis.
2. Low Levels of EPO
An acquired mutation in exon 14 of the tyrosine kinase JAK2 is the main defect in nearly 95% of cases of polycythemia vera. (V617F). Exon 12 of JAK2 has also been linked to mutations. These mutations cause JAK2 to lose its auto-inhibitory pseudo-kinase region, causing it to become constitutively active. Due to this constitutive stimulation, the erythroid colony becomes both hypersensitive to EPO and EPO-independent.
Histopathology
Bone marrow testing is not frequently used. Its application is mainly limited to situations where there is a high clinical suspicion of polycythemia vera despite the lack of a JAK2 mutation or when testing facilities are not available. When classic findings are present along with other indicative haematology parameters, polycythemia vera is more likely to be diagnosed.
Hyper-cellular marrow with erythroid hyperplasia and subtle megakaryocytic atypia are among the results that are highly suggestive. Another anticipated characteristic is tri-lineage hyper-proliferation.
Common symptoms
- Common presenting symptoms of transient ischemic attacks include exhaustion, headache, vertigo, momentary blurry vision, amaurosis fugal, and other generally non-specific symptoms. (TIAs).
Rarely, patients may experience pruritus after taking a tepid shower, especially on the back.
- Epistaxis, GI haemorrhage, or easily bruised skin may be present in the past.
- Patients with peptic ulcer disease frequently also have non-specific abdominal discomfort. Early satiety and left hypochondriac discomfort should raise the possibility of splenomegaly.
- Rarely, patients may report having experienced inexplicable thrombotic complications like digital infarcts or Budd-Chari syndrome.
In patients with congenital cardiac disease, it is crucial to try and extract aetiology-specific history, such as a history of smoking, a prolonged stay at a high altitude, and congenital cardiac disease.
Physical examination
- There may be obvious abnormal face ruddiness.
- Cyanosis, clubbing, and the detection of a murmur during auscultation all point to a hereditary cyanotic heart condition.
- Even in a non-committal patient, nicotine staining of the teeth and nails constitutes presumptive proof of smoking.
- A barrel chest could indicate obstructive lung disease, while morbid obesity could raise the chance of the Pickwickian syndrome.
- A visible spleen or the bruit of renal arterial stenosis in a thin-built.
person may be found during an abdominal examination.
Evaluation
A process of assessment must be sequential. It is crucial to take into account the appropriate inquiry in that particular clinical context due to the wide range of possible causes.
Hemogram
Hematocrit values above 49% for men and 48% for women at sea level are to be regarded as suggestive of polycythemia vera according to the WHO 2017 criteria. Leukocyte and platelet counts may also rise at the same time as polycythemia vera instances. Eosinophilia and basophilia may be present along with a leucocyte count that is typically between 10,000 and 20,000/micrometre. Rarely will platelet counts surpass 1,000,000 per microliter.
Radioisotope Research
Chromium-labelled autologous RBC transfusions are used in radioisotope studies to precisely calculate the real RBC mass and definitively rule out fictitious polycythemia.
Levels of Serum EPO:
The further evaluation strategy is guided by the presence of either high or low EPO levels.
- Low Levels of EPO
Primary polycythemia is indicated by low EPO levels. The goal of a subsequent assessment should be to find polycythemia vera.
- High levels of EPO
Secondary polycythemia is indicated by high EPO levels. The reason should be ascertained through further analysis. This should contain the following, but not only:
- Using a pulse oximeter to measure arterial oxygen saturation levels: low levels are likely indicative of a heart or pulmonary cause.
- Additional analysis may be necessary for normal saturation levels, for example: a co-oximeter is used to rule out methemoglobinemia.
- measuring smokers' amounts of carboxyhemoglobin. Hb P50 measurement to identify high affinity hemoglobinopathies. studies necessary to identify a potential tumour that secretes EPO
Serum Levels of Folate, Vitamin B12, and Ferritin
Low folate and low blood ferritin levels have been more frequently linked to primary polycythemia. [4] Increased amounts of vitamin B12, often startling, may be seen. Leukocytes' greater secretion of transcobalamin III is the cause of this.
Evaluation of Renal Function
Abnormal renal function raises the possibility of secondary polycythemia. Because of increased cell proliferation and following turnover, uric acid levels are frequently raised.
Evaluation of Hepatic Status
Secondary polycythemia and higher RBC proliferation have been linked to liver cirrhosis and inflammatory liver disease.
Ultrasound
An ultrasound and Doppler study of the abdomen would help identify a secondary cause.
In cases of suspected secondary polycythemia, the utility of additional investigations such as a chest radiograph, lung function tests, sleep studies, and an echocardiograph are to be considered as appropriate.
Treatment/Management
The treatment of secondary polycythemia is directed at correcting the cause.
For polycythemia vera, available treatment modalities include:
Phlebotomy
Phlebotomy was established as the backbone of therapy, primarily based on the trial conducted by the Polycythemia Vera Study Group (PVSG). The study found that, compared to chlorambucil or radioactive phosphorous treatment, treatment with phlebotomy alone was associated with longer median survival.
The rationale behind repeated phlebotomies was that cytoreduction would reduce hyper-viscosity. Additionally, it would induce a state of iron deficiency that would help retard red cell proliferation
Phlebotomy is typically designated for the following conditions for secondary polycythemias:
- recurring pulmonary conditions
- Cyanotic cardiac conditions
- Patients who have undergone a kidney transplant and have hypertension and erythrocytosis but do not react to ACEIs or angiotensin receptor blockers at the recommended doses (ARBs).
Hydroxyurea
Typically, hydroxyurea is regarded as a second-line treatment. The Polycythemia Vera Study Group (PVSG) study, which revealed reduced rates of thrombosis compared to a historical cohort treated with phlebotomy alone, was one source of benefit evidence. Despite theoretical worries, studies have not discovered a conclusive link between hydroxyurea use and a higher chance of leukemic transformation.
Use indications include:
- inadequate vein entry
- High testing standards
- when logistical issues make sampling impossible
- significant thrombocytosis
- Uncontrollable itch
- The usual doses per day vary from 500 to 1500 mg.
- Target platelet numbers below 500,000/mcL by adjusting doses. To ensure that the absolute neutrophil count stays above 2000/microliter, dosages must be changed.
Aspirin Low-Dose
Even though they lived longer, patients who received only phlebotomy treatment had a higher risk of getting thrombosis in the first three years of treatment, according to the original PVSG trial. This seemed to imply a possible advantage of using anti-platelet or anticoagulant medications simultaneously. First-round studies with higher aspirin or dipyridamole doses revealed poor gastrointestinal haemorrhage. However, later research revealed that lower aspirin doses could be used securely.
Aspirin is currently recommended when other cardiovascular risk factors are present or when there is insufficient control of microvascular symptoms after reaching the goal hematocrit. When necessary, it is advised to take aspirin in low amounts of 40 to 100 mg per day
Control of Pruritus
Antihistamines and selective serotonin reuptake inhibitors are examples of therapeutic modalities that are accessible for symptomatic relief, depending on the severity of pruritus and the clinical reaction to therapy. (SSRIs).
Pregnancy and the Treatment of Polycythemia Vera
In most cases, phlebotomy and low-dose aspirin are suitable standard therapeutic measures. Pegylated interferon (IFN-alpha) may also be necessary for some high-risk female patients.
The treatment of new-born polycythemia
Most people don't require medical attention. Hyper-viscosity can rarely necessitate exchange transfusion.
Differential diagnosis
- First-stage myelofibrosis
- myeloid leukaemia persistent
- thrombocythemia vital
- changes in the EPO receptor
Prognosis
According to studies, there is a 14.1-year median lifetime for people with polycythemia vera.
Better prognosis was discovered to be correlated with the following factors:
- Thrombocytosis
- Pruritus: It was not obvious why pruritus was associated with a better prognosis. This might be explained by the following:
- Patients with significant pruritus were more likely to seek medical attention sooner due to the lead-time bias.
- Decreased danger of vascular thrombosis
Complications
Hyper-viscosity-related complications are mainly linked to secondary polycythemia. The complications of polycythemia vera include a higher chance of thrombosis and the development of malignant conditions.
The following problems are frequently seen:
- Bleeding: It's common to experience recurrent epistaxis or gastrointestinal bleeding, which can cause iron deficiency anaemia and possibly skew clinical results like how the bone marrow looks
- thrombus: Both arterial and venous thrombus are more common because of hyper-viscosity. Digital infarcts and brain ischemic infarcts are signs of arterial thrombosis, especially in areas near watersheds. It's also common to see venous thromboembolism, including Budd-Chari syndrome.
- Acute myeloid leukaemia (AML) progresses to leukaemia in about 5% of cases and is frequently resistant to therapy.









