Polycythemia vera is a type of blood cancer that belongs to a group of conditions known as myeloproliferative neoplasms (MPNs). MPNs are a group of disorders characterised by the overproduction of one or more types of blood...
Introduction:
- Polycythemia vera is a type of blood cancer that belongs to a group of conditions known as myeloproliferative neoplasms (MPNs). MPNs are a group of disorders characterised by the overproduction of one or more types of blood cells, including red blood cells, white blood cells, and platelets.
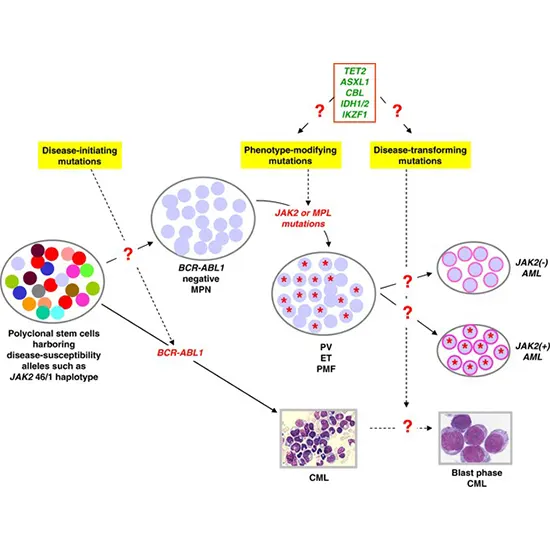
- Other types of MPNs include essential thrombocythemia and primary myelofibrosis. All MPNs are caused by mutations in the genes that control blood cell production. These mutations cause the bone marrow to produce too many blood cells, leading to an increase in the number of blood cells in the bloodstream.
Causes of polycythemia vera and other MPNs:
A collection of uncommon blood disorders known as myeloproliferative neoplasms (MPNs), including polycythemia vera (PV), are characterised by the overproduction of one or more blood cell types in the bone marrow. Although the precise causes of these conditions are not fully known, number of variables are thought to play a role in their emergence.
- Gene mutations: A genetic mutation that affects the generation of blood cells is present in the bulk of patients with PV and other MPNs. Patients with these diseases frequently have mutations in genes like JAK2, CALR, and MPL.
- Environmental factors: The risk of getting MPNs may be increased by exposure to some environmental toxins, including benzene, radiation, or specific chemicals.
- Age: The average age at diagnosis for PV and other MPNs is in the 60s, with older people having a higher prevalence.
- Family history: The likelihood of getting an MPN may be increased if you have a first-degree relative (such as a parent or sibling) who has the illness.
- Other medical conditions: Autoimmune disorders and chronic infections are two conditions that may raise the risk of getting MPNs.
Aggravating factors:
- Things that can make a specific disease or circumstance worse or more severe are referred to as aggravating factors. A few examples of aggravating factors in the setting of health are:
- High amounts of stress can make number of health conditions worse, including physical conditions like high blood pressure and chronic pain as well as mental health conditions like anxiety and depression.
- Obesity, diabetes, and heart disease are just a few of the health issues that can be brought on by a poor diet that is high in packaged foods, sugar, and saturated fat.
- Lack of exercise: A sedentary lifestyle can lead to obesity, bad cardiovascular health, weakened musculature, and broken bones, among other health issues.
- Environmental factors: Asthma, allergies, and autoimmune diseases can all become worse when people are exposed to pollutants, allergens, and other environmental poisons.
- Abuse of substances: Abuse of substances, such as alcohol and drugs, can make a number of health conditions worse, such as heart disease, liver disease, and mental health conditions.
- Unhealthy sleep: Chronic sleep loss or unsatisfactory sleep can make a number of medical conditions worse, such as mental health problems, obesity, and cardiovascular disease.
- In order to successfully manage and treat health conditions, it is crucial to recognise and address aggravating factors. Self-care, getting medical attention, and altering one's lifestyle can all help to lessen the negative effects of aggravating factors on health.
Symptoms of Polycythaemia vera and other MPNs:
- Depending on the particular MPN and the severity of the condition, the symptoms of polycythemia vera (PV) and other myeloproliferative neoplasms (MPNs) can change. The following are some of the most prevalent MPN symptoms:
- Weakness and fatigue: People with MPNs frequently experience weakness and fatigue, which can affect their everyday activities.
- Breathing difficulties: MPNs can increase the amount of red blood cells in the body, which can cause the blood to thicken and make breathing difficult.
- Increased blood viscosity has been linked to migraines, lightheadedness, and confusion.
- Vision issues: Vision issues, such as double vision, blurred vision, and blind areas, can be brought on by thickened blood.
- Lymph node swelling: MPNs can cause lymph nodes to enlarge, especially in the armpit and neck regions.
- Abdominal discomfort and pain: MPNs can result in an enlarged spleen, which can produce early satiety and abdominal discomfort and pain.
- Skin itch: MPN patients may experience skin itch, particularly after a warm bath or shower.
- Bruising and bleeding: MPNs occasionally cause bruising and bleeding, even with small wounds.
- Sweating excessively while sleeping can be a sign of an MPN.
- Bone pain: MPNs can, in uncommon circumstances, result in bone pain or fractures.
Familial relationships:
ties within a family, such as those between parents, children, siblings, grandparents, aunts, uncles, and cousins, are referred to as familial ties. Here are a few instances of family ties:
- A parent's (mother or father) and child's connection is known as the parent-child relationship. A mother and daughter, a father and son, or a parent raising their kid alone are some examples.
- Brothers and/or women who are related by blood are said to be siblings. Sisters and brothers, twins, and half-siblings are a few examples.
- A collection of diseases known as myeloproliferative neoplasms (MPNs), which include polycythemia vera (PV), affect the bone marrow and result in an excessive production of blood cells. The majority of the time, MPNs are sporadic, which means they are not passed down through families or hereditary. Rarely, MPNs may be familial, which means that acquired genetic mutations are their primary cause.
- JAK2, CALR, and MPL are just a few of the genetic changes that have been connected to MPNs. These mutations may occasionally be handed down from parents to their offspring, increasing the risk of MPN development.
- It is crucial to remember that even if a person gets a genetic mutation connected to MPNs, it does not mean they will inevitably become ill with the condition. Although the presence of the mutation may raise their risk, other variables that affect MPN development include environmental exposures and lifestyle choices.
- It may be advised that other family members undergo genetic testing to see if they have inherited a mutation related to the disease if one member of the family has been diagnosed with an MPN. This can aid in the condition's early discovery, monitoring, and decision-making regarding family planning.
Environmental influences:
- Environmental variables also play a role in the development of myeloproliferative neoplasms like polycythemia vera (PV) and other MPNs. Environmental elements that have been linked to the emergence of MPNs include:
- Radiation exposure: Ionising radiation exposure has been associated with the development of MPNs, particularly in people who have received radiation treatment for a prior cancer or who have worked in environments with high levels of radiation exposure.
- Chemical exposure: It has been established that exposure to specific chemicals, such as benzene and other solvents, increases the risk of getting MPNs.
- Infections: Hepatitis C and the human T-cell leukaemia virus type 1 (HTLV-1) have both been associated with a higher chance of developing MPNs.
- Lifestyle factors: MPN development has also been linked to smoking, obesity, and a lack of physical exercise.
- It is crucial to remember that not everyone who is exposed to these environmental factors will acquire an MPN, and that there is a complicated and poorly understood link between environmental factors and MPNs. Individuals who have been exposed to these factors should be conscious of their potential risk, though, and take precautions to reduce it whenever they can. For people who have a higher risk of getting an MPN because of environmental factors, routine medical exams and screening tests may also be advised.
Dietary Effects:
It is unclear how diet affects the onset of polycythemia vera (PV) and other myeloproliferative neoplasms (MPNs), and more study is required to ascertain whether any dietary elements contribute to the onset or progression of these conditions. However, the following dietary elements have the ability to affect MPNs:
- Consumption of iron: PV is characterised by an excessive production of red blood cells, which raises the risk of blood blockages. Individuals with PV are frequently recommended to avoid iron supplements and restrict their intake of iron-rich foods, such as red meat and fortified cereals, because excessive iron intake can increase the risk of blood clots.
- The omega-3 fatty acids, which are present in fatty fish, flaxseed, and walnuts, may have a protective impact against MPNs, according to some research. To prove this connection, more study is required.
- Alcohol: Because drinking excessive amounts of alcohol has been associated with an increased chance of MPNs, including PV, people with these conditions are frequently advised to cut back on or completely avoid alcohol.
- Obesity: Maintaining a healthy weight through a balanced diet and consistent exercise may be advantageous for people with MPNs because obesity has been linked to an increased chance of developing MPNs.
Overall, no dietary strategy or nutrient has been proven to be associated with the prevention or therapy of MPNs. The maintenance of a balanced diet, however, can be advantageous for general health and may assist those who have MPNs in managing their symptoms and lowering their risk of complications.
Diagnosis of Polycythaemia vera and MNPs:
A mix of physical examination, blood tests, and bone marrow biopsy are used to diagnose polycythemia vera.
- Physical inspection: A healthcare professional will conduct a physical examination to check for polycythemia vera signs and symptoms, such as high blood pressure, an enlarged spleen, and skin redness.
- Blood tests: The first blood test usually ordered to check for polycythemia vera is a complete blood count (CBC). A CBC counts the quantity of platelets, white blood cells, and red blood cells in the blood. The red blood cell count is typically greater than average in polycythemia vera. In addition to genetic testing to check for mutations linked to polycythemia vera, additional blood tests may be required to evaluate the health of the kidneys and the liver.
- Bone marrow biopsy: During a bone marrow biopsy, a tiny sample of bone marrow is taken for examination. This test can confirm the polycythemia vera diagnosis and clear out other illnesses that might present with comparable symptoms. To search for abnormal cells and gauge the quantity of red blood cells in the bone marrow, the sample is examined under a microscope.
- A thrombophilia panel, which can detect genetic mutations that raise the risk of blood clots, may be performed in order to assess for polycythemia vera complications such as blood clotting disorders.
- Healthcare professionals will assess patients for other myeloproliferative neoplasms (MPNs), a collection of blood cancers that share many similarities with polycythemia vera, in addition to the diagnosis of polycythemia vera. These include primary myelofibrosis and essential thrombocythemia, which also have an excess of blood cells and a higher chance of blood clots.
Overall, a thorough examination by a medical professional is necessary to make the diagnosis of polycythemia vera, and it may also entail a number of tests to identify the condition and rule out other possible causes of symptoms.
Precautions need to take:
For individuals with polycythemia vera and myeloproliferative neoplasms (MPNs), the following precautions can be taken:
- routine check-ups: Patients with polycythemia vera and MPNs should visit their doctors for routine check-ups on a regular basis. This can assist in tracking the disease's development, spotting any possible complications, and modifying the treatment strategy as necessary.
- Compliance with medication: Polycythemia vera and MPN patients may be given drugs to regulate blood cell production and avoid complications like blood clots. Patients should take these medicines exactly as directed and let their doctor know right away if they experience any side effects.
- Avoid smoking: Smoking can increase the chance of polycythemia vera complications.
Various treatment options:
- For polycythemia vera and myeloproliferative neoplasms (MPNs), there are number of treatment choices, including the following:
- Phlebotomy: Phlebotomy is the removal of blood from the body in order to decrease the amount of red blood cells. This can lessen polycythemia vera signs and lower the possibility of complications.
- Drugs: Drugs can be used to regulate the creation of blood cells and stop problems like blood clots. These could include ruxolitinib, interferon-alpha, hydroxyurea, ibuprofen, and so forth.
- Transplantation of the bone marrow: For some patients with polycythemia vera and MPNs, a bone marrow transplant may be a possibility. This entails using healthy bone marrow from a stranger to replace the patient's own bone marrow.
- Radiation therapy: Radiation therapy is a treatment option for spleen enlargement, a frequent MPN side effect.
- Chemotherapy: Chemotherapy can be used to treat advanced MPN cases or as a pre-transplant preparation medication.
- Targeted therapy is a form of medical intervention that specifically targets molecules involved in the development and spread of cancer cells. This could apply to medications like imatinib, which is used to treat chronic myeloid leukaemia and attacks the BCR-ABL protein. (CML).
- Clinical trials: Research studies that evaluate novel polycythemia vera and MPN therapies individually or in combination. If a patient satisfies certain requirements, they may be qualified to take part in clinical studies.
The patient's symptoms, age, general health, and other variables influence the treatment option for polycythemia vera and MPNs. To create a unique treatment strategy that considers each patient's requirements and objectives, patients and their healthcare provider should collaborate closely.
As a result of an excessive production of red blood cells, Polycythemia vera is an uncommon form of blood cancer. Despite being a chronic, incurable disease, it can be successfully managed with a range of therapeutic approaches, including phlebotomy, drugs, bone marrow transplant, radiation therapy, chemotherapy, targeted therapy, and clinical trials. In order to avoid complications and enhance the quality of life for patients with this disease, early diagnosis and treatment are crucial. Additionally, it's critical for patients to practise preventative measures like routine check-ups, drug compliance, staying hydrated, quitting smoking, and stress management. Patients with polycythemia vera can manage their condition and lead fulfilling lives by working closely with their healthcare practitioner and adhering to these recommendations.









