Many facets of human health and illness are significantly influenced by genetics. Our physical characteristics, behavioural characteristics, and susceptibility to certain illnesses are all influenced by the instructions found...
Leiomyosarcoma (LMS) is a form of cancer that develops from smooth muscle cells, which can be found in the uterus, stomach, intestines, blood vessels, skin, and other bodily organs and tissues.
Less than 5% of all soft tissue sarcomas are LMS, an uncommon form of cancer. Although LMS can happen at any age, people over the age of 50 are more likely to develop it.
Although the precise origin of LMS is unknown, it is believed to be linked to genetic changes and mutations in the smooth muscle cells that cause uncontrolled cell development and division.
Possible Reasons for Leiomyosarcomas
Although the precise causes of leiomyosarcoma (LMS) are not completely understood, there are a number of things that may have an impact on how it develops:
- Genetic mutations: LMS may develop as a result of modifications to the DNA of smooth muscle cells, which could contribute to uncontrollable growth and division.
- Age: LMS is more prevalent in people over the age of 50, which implies that getting older could be a risk factor. High levels of radiation exposure, such as those experienced during cancer treatment, may raise the chance of developing LMS.
- Gender: Women are more prone than men to develop leiomyosarcoma, particularly when it involves the uterus.
- Radiation exposure: Ionising radiation exposure, such as that experienced during radiation therapy or cancer treatment, may raise the chance of developing leiomyosarcoma.
- Chemical exposure: Being exposed to some chemicals, like vinyl chloride or arsenic, may make you more likely to get leiomyosarcoma.
- Immunosuppression: Those with impaired immune systems, such as those with HIV/AIDS or organ transplant recipients, may be more susceptible to leiomyosarcoma.
It is crucial to remember that a person does not necessarily have to have one or more of these risk factors in order to develop leiomyosarcoma; in fact, some individuals who get this cancer have no known risk factors.
Role of Genetics
Many facets of human health and illness are significantly influenced by genetics. Our physical characteristics, behavioural characteristics, and susceptibility to certain illnesses are all influenced by the instructions found in our genes. Changes in the DNA sequence of our genes, known as genetic mutations, can directly cause some illnesses or raise the risk of getting others.
Genetic mutations that are passed down through the parents:
- Some genetic mutations can increase the risk of developing a particular illness or disorder. Huntington's disease, sickle cell anaemia, and cystic fibrosis are a few examples of hereditary genetic mutations.
- Genetic mutations that emerge randomly during cell division are referred to as spontaneous mutations because they do not come from a parent. Numerous illnesses, including cancer, can be brought on by spontaneous mutations.
- Single nucleotide polymorphisms (SNPs), which are minute differences in our genes, can also have an impact on health. These variations may alter the way certain drugs or nutrients are metabolised by our bodies or raise the chance of contracting diseases like diabetes or heart disease.
- Epigenetics: Alterations in epigenetic material can also affect health. The term "epigenetics" describes changes in gene expression or activity that are not brought on by modifications to the DNA structure. Epigenetic changes can have an impact on health and are brought on by environmental variables like diet, stress, and exposure to toxins.
Genetic testing can assist in locating genetic changes or mutations that might raise a person's risk for developing a particular illness, enabling early diagnosis and treatment. Genetic research is also improving our knowledge of the underlying causes of many illnesses and assisting in the development of novel therapies.
Role of Family History
- Family history, including leiomyosarcoma, can be a major risk factor for developing some cancers. The chance of getting this kind of cancer can occasionally be increased by a genetic mutation that runs in families.
- For instance, a rare genetic disease called hereditary leiomyomatosis and renal cell cancer (HLRCC) raises the chance of getting leiomyosarcoma as well as other cancers. Mutations in the FH gene, which creates an enzyme that aids in cell energy production, are the cause of HLRCC. HLRCC patients are more likely to acquire kidney cancer, skin tumours, other types of smooth muscle tumours, and uterine leiomyosarcoma.
- Leiomyosarcoma risk may also be increased by other genetic mutations, though these are still poorly known. It may be advised to undergo genetic testing and counselling in instances where there is a significant family history of leiomyosarcoma or other cancers in order to look for any genetic mutations that might be increasing the risk.
- It's crucial to remember that the majority of leiomyosarcoma instances do not result from inherited genetic mutations and develop sporadically, which means they are not connected to a family history of the condition.
Who is More Prone?
leiomyosarcoma can be influenced by a number of factors, including:
- Prior radiation exposure: Leiomyosarcoma risk is increased by radiation exposure at large doses, such as during radiation therapy or cancer treatment.
- Certain genetic mutations: Hereditary leiomyomatosis and renal cell cancer are two examples of inherited genetic mutations or changes in DNA that increase the chance of developing leiomyosarcoma. (HLRCC).
- Chemical exposure: Being exposed to some chemicals, like vinyl chloride or arsenic, may make you more likely to get leiomyosarcoma.
- Immune system weakness: Those with HIV/AIDS or organ donation recipients who have immune systems that are already compromised may be more susceptible to leiomyosarcoma.
Symptoms Patient Encounters With:
While some leiomyosarcoma patients may not initially exhibit any signs, others may do so in a variety of ways. Leiomyosarcoma signs frequently seen include:
- Leiomyosarcoma's most prevalent symptom is pain, which may be restricted to the tumour's region or more generalised.
- Growth: If the tumour is close to the skin's surface, you might feel a lump or growth there.
- Weakness or lethargy may be a symptom of leiomyosarcoma, especially if the tumour is the source of anaemia. (low red blood cell count).
- Weight loss: Some people with leiomyosarcoma may experience unexplained weight loss, especially if the tumour is advanced.
- Leiomyosarcoma can occasionally result in fever, especially if it has spread to other areas of the body. Changes in bowel or bladder function may result from the tumour's pressure on adjacent organs if it is in the abdomen or pelvis.
It's important to remember that these symptoms can be brought on by a variety of different diseases, so just because someone exhibits one or more of them doesn't necessarily indicate they have leiomyosarcoma. However, it's crucial to speak with your doctor if you are exhibiting any of these signs or are worried about your health in order to identify the underlying issue and receive the proper care.
Prevalence of Leiomyosarcomas
- Less than 1% of adult cancers are leiomyosarcomas, an uncommon form of cancer. The location of the tumour affects the frequency of leiomyosarcoma.
- The most prevalent form of leiomyosarcoma, accounting for 1% to 2% of all uterine tumours, is uterine leiomyosarcoma. It is uncommon in women under the age of 30 and is most frequently found in postmenopausal women.
- Leiomyosarcoma can also develop in the blood vessels, retroperitoneum (the region behind the abdominal cavity), and gastrointestinal system. Men are more likely to develop retroperitoneal leiomyosarcoma than women, and older people are more likely to develop gastrointestinal leiomyosarcoma.
- There is no known lifestyle factor that increases the risk of getting leiomyosarcoma, and the precise cause of the disease is unknown. However, some DNA changes or genetic mutations may raise the risk of getting leiomyosarcoma, especially in people with a family history of the condition.
Screening Test for Leiomyosarcomas
Depending on where the tumour is located and how the patient is feeling, different tests may be required to identify and quantify the spread of leiomyosarcoma. However, some of the fundamental to sophisticated procedures that could be requested include:
- Physical examination: To look for lumps or swelling in the affected region, the doctor may perform a physical examination.
- Imaging tests: To help visualise the tumour and ascertain its position and size, imaging tests such as X-rays, CT scans, MRI scans, or ultrasound may be prescribed.
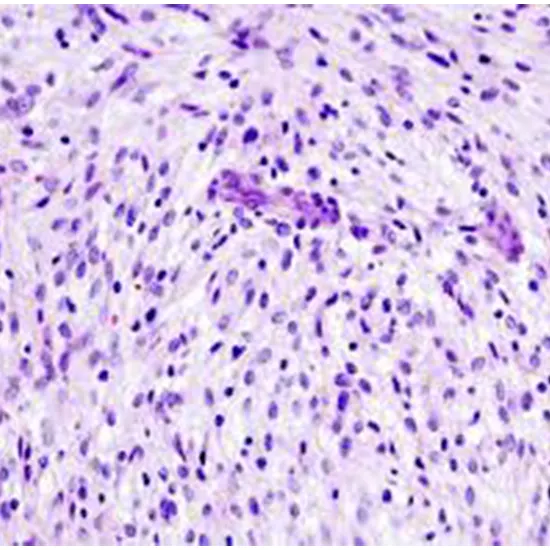
- A biopsy entails taking a sample of the tumour tissue for laboratory examination. By doing so, it will be possible to identify the precise type of leiomyosarcoma and validate the diagnosis.
- Blood tests: Blood tests can be used to assess the health of important organs and look for any indications of inflammation or illness that might be related to a tumour.
- Using a PET scan, a specialist imaging test, it is possible to locate any bodily parts where the cancer may have spread.
- Molecular testing: Molecular testing examines the tumour cells' DNA to find any particular hereditary mutations that might be connected to the tumour. This can assist in deciding which treatment strategy is ideal for the particular patient.
In order to fully assess the extent of the tumour and choose the most appropriate course of treatment, the doctor may order additional tests as required. It is essential to note that the specific tests ordered may differ based on the circumstances of each individual case.
Various Stages of Leiomyosarcoma
Typically, the American Joint Committee on Cancer (AJCC) TNM staging method is used to stage leiomyosarcoma. This method considers the tumour's size (T), whether the cancer has metastasized (M) to distant organs, and whether it has spread to adjacent lymph nodes (N). The various phases of leiomyosarcoma are as follows:
- Stage I: The tumour is smaller than 5 cm in size and is confined to the organ or tissue from which it started.
- Stage II: The tumour is larger than 5 cm in size but is still confined to the organ or tissue from which it started.
- Stage III: The tumour has spread to adjacent lymph nodes and may or may not have penetrated nearby tissues or structures, such as bone or blood vessels.
- Stage IV: The tumour has spread to remote organs like the liver or lungs.
The prognosis and available treatments will vary depending on the position and size of the tumour, cancer's stage, and the patient's general health, so it is challenging to determine which stage of leiomyosarcoma is "safe." No matter what stage the cancer is in, getting therapy and early detection is crucial for the best results.
Various Treatment Options
The available treatments for leiomyosarcoma may vary depending on the position, size, and extent of the tumour as well as the patient's general health. Chemotherapy, radiation therapy, and surgery are the three main leiomyosarcoma treatments.
- Surgery is typically the first line of defence against leiomyosarcoma. Surgery aims to completely eliminate the tumour as well as any nearby tissue that has been harmed. The surgeon may conduct a wide local excision (removal of the tumour and surrounding tissue) or a radical resection depending on the size and position of the tumour. (removal of the entire organ). If the tumour is in a bone or soft tissue that cannot be completely removed, an amputation of a leg may occasionally be required.
- High-energy radiation is used in radiation treatment to kill cancer cells. Before or after surgery, radiation treatment can be used to shrink the tumour and eradicate any cancer cells that may still be present. In some circumstances, it may also be used to treat complaints like pain.
- Chemotherapy: Drugs are used in chemotherapy to eradicate cancer cells. It can be used to reduce the tumour before surgery or to eradicate any cancer cells that may still be present after surgery. In advanced instances where the tumour has spread to other body parts, chemotherapy may also be used to treat symptoms.
- Targeted therapy is a form of medical care in which drugs are used to specifically target particular proteins or genetic mutations in cancer cells. In some instances of leiomyosarcoma, targeted therapy may be used, especially if the tumour carries particular genetic mutations that can be targeted by specific medications.
- Immunotherapy: An approach to treating disease that makes use of the immune system of the patient's body. In some instances of leiomyosarcoma, this type of therapy may be used, especially if the tumour carries particular genetic mutations that can be targeted by specific immunotherapy medications.
The stage and size of the tumour, the patient's general health, and the preferences of the patient and medical staff will all affect the course of therapy for leiomyosarcoma. To obtain the best results, treatment plans may incorporate a combination of these therapeutic modalities.
Prognosis of Leiomyosarcoma
- The prognosis for leiomyosarcoma relies on a number of variables, including the tumour's size and location, cancer's stage, its grade, the patient's age and general health, and the effectiveness of the treatment.
- Leiomyosarcoma is cancer that is regarded as being comparatively aggressive, and its prognosis is typically worse than that of some other sarcomas. Depending on cancer's stage, the 5-year survival percentage for those with leiomyosarcoma varies. The 5-year survival statistics for leiomyosarcoma, broken down by stage, are as follows:
- stage: roughly 64%
- stage two: roughly 56%
- Stage III: 39%
- Stage IV: 14%
- It's crucial to keep in mind that these survival numbers are based on population data and might not accurately represent each patient's personal prognosis. Depending on their particular situation, some individuals might experience a better or worse outcome.
- Leiomyosarcoma's size and location of the tumour, the cancer's stage, the presence of metastases, and the tumour's grade are all variables that could suggest a poor prognosis. Patients should talk with their medical team about their unique prognosis and treatment choices.
Leiomyosarcoma is a rare and aggressive type of soft tissue cancer that poses major diagnostic and therapeutic challenges. Patients with this illness still have a poor prognosis despite advances in medical science. However, there is hope for a better future by increasing awareness and funding the ongoing studies. We can continue to advance our knowledge of and access to more potent treatments for this devastating condition by working together as patients, healthcare workers, and scientists.









