Primary hyperparathyroidism, an ailment in which the parathyroid glands yield too much parathyroid hormone (PTH), is the most common cause of hypercalcemia. This condition affects approximately 1 in 500 people, with a majority...
A closer look at hypercalcemia - Introduction
High levels of calcium (Ca2+) in the blood serum are referred to as hyperglycemia.
Hypercalcemia is characterized by levels higher than 2.6 mmol/L, which are outside the normal range of 2.1-2.6 mmol/L (8.8-10.7 mg/dL, 4.3-5.2 mEq/L).
Know the prevalence - protect yourself against this condition - Epidemiology.
The epidemiology of hypercalcemia varies depending on the underlying cause of the condition.
Prevalence
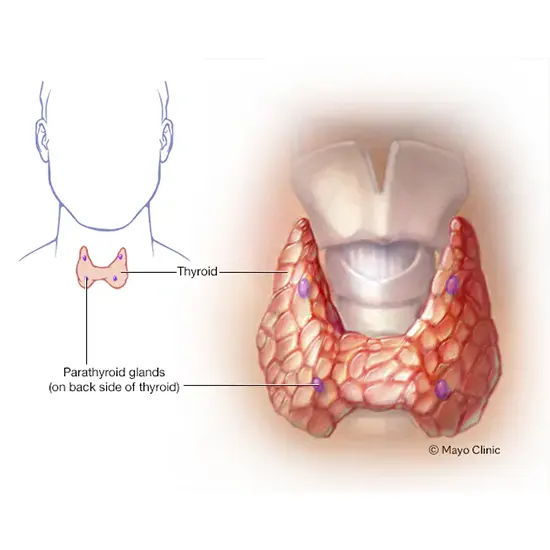
Primary hyperparathyroidism, an ailment in which the parathyroid glands yield too much parathyroid hormone (PTH), is the most common cause of hypercalcemia. This condition affects approximately 1 in 500 people, with a majority in women and older adults.
Other causes of hypercalcemia, such as cancer or certain medications, are less common but can still occur. The prevalence of hypercalcemia in cancer patients varies depending on the type of cancer, with some types such as multiple myeloma having a higher risk of hypercalcemia. Certain medications, such as thiazide diuretics and lithium, can also cause hypercalcemia.
Overall, hypercalcemia is more common in older adults and individuals with a history of cancer or certain medical conditions. Women suffer more than men.
Incidence
The incidence of hypercalcemia is difficult to determine due to the various underlying causes and the fact that many cases of mild hypercalcemia may go undiagnosed. However, it is crucial to be familiar with the risk factors for hypercalcemia and to seek medical attention if symptoms occur.
Understanding the pathogenesis of this condition is the first step to finding a cure.
Let's talk about pathogenesis
Hypercalcemia can result from a variety of mechanisms that disrupt the normal balance of calcium metabolism in the body. Primary hyperparathyroidism is the most crucial factor, this occurs when the parathyroid glands produce too much parathyroid hormone (PTH). In the intestines, PTH promotes calcium absorption, calcium reabsorption in the kidneys, and calcium release from bone.
Excess PTH causes increased calcium release from bone and decreased calcium excretion by the kidneys, leading to elevated calcium levels in the blood. Other causes of hypercalcemia include certain cancers, such as multiple myeloma and breast cancer, which can release calcium into the bloodstream or produce substances that mimic the action of PTH.
In addition, certain medications, such as thiazide diuretics and lithium, can cause hypercalcemia by increasing calcium reabsorption in the kidneys. Vitamin D toxicity, sarcoidosis, and granulomatous diseases can also lead to hypercalcemia by increasing intestinal absorption of calcium or by promoting calcium release from bone.
Know the Types: Understanding the Different Causes of Hypercalcemia.
Some common types include:
Primary hyperparathyroidism:
This is a condition when the parathyroid glands stimulate much of the parathyroid hormone (PTH), which leads to elevated calcium levels in the blood.
Malignancy-associated hypercalcemia: This type of hypercalcemia is caused by cancers that can produce substances that mimic PTH or promote calcium release from bone, such as multiple myeloma, breast cancer, lung cancer, and some types of lymphoma.
Medication-induced hypercalcemia:
Certain medications, such as thiazide diuretics, lithium, and excessive vitamin D supplements, can cause hypercalcemia by increasing calcium reabsorption in the kidneys or promoting calcium absorption in the intestines.
Vitamin D toxicity:
Excessive intake of vitamin D supplements or overexposure to sunlight can result in hypercalcemia by boosting intestinal absorption of calcium.
Granulomatous diseases:
Sarcoidosis and other granulomatous diseases can cause hypercalcemia by promoting the formation of granulomas, which activate vitamin D and increase calcium absorption in the intestines.
Immobilization:
Prolonged immobilization can cause hypercalcemia by increasing bone resorption and decreasing calcium excretion by the kidneys.
Familial hypocalciuric hypercalcemia:
This is an inherited disorder that affects calcium regulation and causes a mild increase in blood calcium levels.
Milk-alkali syndrome:
This occurs when excessive calcium and antacid intake leads to hypercalcemia.
Exploring the Culprits: Uncovering the Various Causes of Hypercalcemia.
Hypercalcemia can result from a variety of underlying causes, including:
Primary hyperparathyroidism:
This is the most common cause of hypercalcemia and occurs when one or additional of the parathyroid glands stimulate too much parathyroid hormone (PTH). Excess PTH causes increased calcium release from bone and decreased calcium excretion by the kidneys, leading to elevated calcium levels in the blood.
Cancer:
Certain cancers, such as multiple myeloma, breast cancer, lung cancer, and some types of lymphoma, can cause hypercalcemia by releasing substances that mimic the action of PTH or by promoting calcium release from bone.
Medications:
Few pills, such as thiazide diuretics, lithium, and vitamin D supplements in excessive amounts, can cause hypercalcemia by increasing calcium reabsorption in the kidneys or by promoting intestinal absorption of calcium.
Vitamin D toxicity:
Excessive intake of vitamin D supplements or exposure to sunlight can result in hypercalcemia by boosting intestinal absorption of calcium.
Sarcoidosis and other granulomatous diseases:
These conditions can cause hypercalcemia by promoting the formation of granulomas, which activate vitamin D and increase calcium absorption in the intestines.
Hyperthyroidism:
Overactive thyroid glands can cause hypercalcemia by increasing bone turnover and releasing calcium into the bloodstream.
Immobilization:
Prolonged immobilization can cause hypercalcemia by increasing bone resorption and decreasing calcium excretion by the kidneys.
Other rare causes:
Familial hypocalciuric hypercalcemia, an inherited disorder that affects calcium regulation, and milk-alkali syndrome, a condition that can occur with excessive calcium and antacid intake can also cause hypercalcemia.
Early intervention is key - be aware of signs - signs and symptoms.
Few signs and symptoms that may occur in individuals with hypercalcemia:
Digestive Symptoms:
Nausea, vomiting, abdominal pain, and constipation are common symptoms of hypercalcemia.
These symptoms may be caused by the effect of calcium on the digestive system.
Renal Symptoms:
Surplus calcium in the blood can injure the kidneys, directing to kidney stones, kidney failure, and increased urine output.
Symptoms may include painful urination, blood in the urine, and increased urination.
Musculoskeletal Symptoms:
Hypercalcemia can cause muscle weakness, fatigue, bone pain, and fractures.
These symptoms may occur because of calcium on muscle and bone tissue.
Neurological Symptoms:
Hypercalcemia can cause confusion, lethargy, depression, and other cognitive changes.
This may be due to the consequence of calcium on the nervous system.
Cardiac Symptoms:
Hypercalcemia can lead to an irregular heartbeat, which can cause palpitations, dizziness, and fainting.
Take the Risk or Lose the Chance: Navigating Life's Uncertainties - Risk factors.
Several risk factors are associated with this condition including:
Hyperparathyroidism:
Hyperparathyroidism is the extensively familiar reason for hypercalcemia. It is a situation in which these parathyroid glands produce too much parathyroid hormone, which leads to an increase in calcium levels in the blood.
Cancer:
Varieties of cancer, such as breast cancer, lung cancer, and multiple myeloma, can cause hypercalcemia. Cancer cells can produce substances that increase calcium levels in the blood.
Medications:
Some medications, such as thiazide diuretics, lithium, and some forms of vitamin D, can cause hypercalcemia.
Immobility:
Prolonged immobility or bed rest can cause hypercalcemia. This is because when the body is inactive, calcium is released from the bones into the blood.
Kidney problems:
The kidneys play a crucial role in regulating calcium levels in the blood. If the kidneys are not well, they may not be able to excrete excess calcium, leading to hypercalcemia.
Dehydration:
When the body is dehydrated, calcium levels in the blood can increase due to a decrease in the amount of fluid available to dilute the calcium.
Empowering patients through accurate diagnosis.
Here are some steps that are typically taken to diagnose hypercalcemia:
Physical exam:
Your physician will perform a physical exam to check for signs of hypercalcemia, such as bone tenderness or abdominal discomfort.
Blood tests:
A blood test is typically the first step in diagnosing hypercalcemia. This will measure the levels of calcium, parathyroid hormone (PTH), vitamin D, and other blood markers that can help identify the underlying cause of hypercalcemia.
Urine tests:
A urine test may also be done to measure the levels of calcium in the urine.
Echoing tests:
Echoing tests such as X-rays, CT scans, or bone scans may be ordered to look for abnormalities in the bones that could be causing hypercalcemia.
Biopsy:
If a tumor or cancer is suspected as the cause of hypercalcemia, a biopsy may be done to confirm the diagnosis.
Treating hypercalcemia with care and expertise - Various treatment options.
The treatment for hypercalcemia depends on the underlying cause and the severity of the condition. In soft cases, therapy may not be essential, and the doctor may simply monitor the calcium levels and symptoms.
Treatment includes:
Fluids:
Increasing fluid intake can help to flush out excess calcium from the body. This is usually the most important treatment for mild hypercalcemia.
Medications:
Several medications can be used to lower calcium levels in the blood. These include bisphosphonates, which help to slow down bone breakdown, and calcitonin, which helps to increase calcium excretion from the kidneys.
Glucocorticoids:
In some cases, glucocorticoids such as prednisone may be used to treat hypercalcemia caused by certain types of cancer.
Surgery:
If hypercalcemia is caused by a tumor, surgery may be necessary to remove the tumor.
Dialysis:
In severe cases of hypercalcemia, dialysis may be necessary to remove excess calcium from the blood.
Healthy Habits Today, Disease-Free Tomorrow.
Here are some tips that can help prevent hypercalcemia:
Stay hydrated:
Adequate hydration is essential for preventing hypercalcemia. Drinking enough fluids can help to flush out excess calcium from the body.
Exercise regularly:
Regular exercise can help to keep bones healthy and prevent bone breakdown, which can lead to an increase in calcium levels.
Manage medications:
If you are taking medications that can cause hypercalcemia, such as thiazide diuretics or vitamin D supplements, make sure to follow your doctor's instructions and monitor your calcium levels regularly.
Manage underlying conditions:
If you have an underlying condition that can cause hypercalcemia, such as hyperparathyroidism or cancer, it's important to work with your healthcare provider to manage the condition and prevent complications.
Get regular check-ups:
Regular check-ups with your healthcare provider can help to detect any changes in calcium levels and identify any underlying conditions that may be contributing to hypercalcemia.
By following these tips, you can help prevent hypercalcemia and maintain good health.
Hope in the Face of Uncertainty: Understanding Prognosis.
Two conditions on which prognosis depends are underlying cause and severity. In most cases, hypercalcemia can be treated effectively, and the outlook is good. However, if not treated or if the condition is severe, hypercalcemia can lead to serious complications.
The severity of hypercalcemia is typically determined by the level of calcium in the blood. Mild hypercalcemia (calcium level between 10.5 and 11.9 mg/dL) is usually not symptomatic and does not instruct therapy. However, moderate (calcium level between 12 and 13.9 mg/dL) or severe (calcium level above 14 mg/dL) hypercalcemia can cause symptoms such as fatigue, muscle weakness, confusion, and even coma.
The underlying cause of hypercalcemia is also an important factor in determining the prognosis. For example, hyperparathyroidism is a common cause of hypercalcemia that can usually be managed effectively with surgery or medications. However, if hypercalcemia is caused by cancer, the prognosis relies on the kind and phase of cancer.
Beware the Risks: Navigating the Complications of Disease.
Some of the possible complications of hypercalcemia include:
Kidney damage:
Excess calcium in the blood can damage the kidneys which further gives rise to kidney stones which may cause kidney failure.
Bone loss:
Hypercalcemia can cause the bones to lose calcium, which is known as osteoporosis, and this boosts the chances of fractures.
Nervous system effects:
Increased blood calcium level affects the nervous system and lead to confusion, lethargy, and even coma.
Heart and blood vessel damage:
Hypercalcemia can cause the heart to work harder, leading to increased pressure of blood and an increased chance of heart attack and stroke.
Gastrointestinal symptoms:
Increased blood calcium levels can cause nausea, vomiting, and constipation.
Dehydration:
Hypercalcemia can cause dehydration due to increased urination.
Increased risk of infections:
Hypercalcemia can weaken the immune system, increasing the risk of infections.









