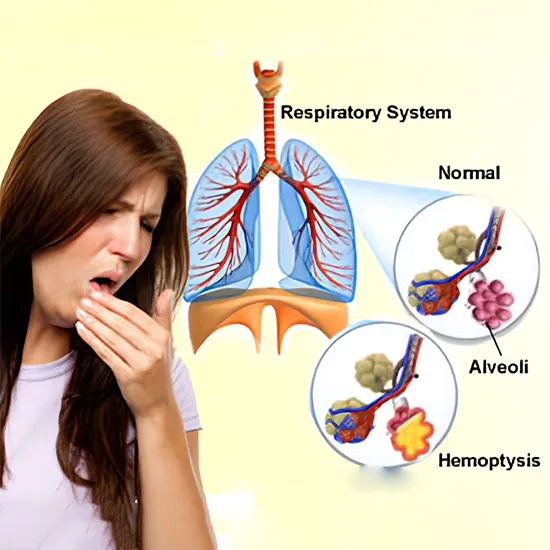
Hemoptysis is characterized by the vomiting of blood originating from the lungs or bronchi as a result of pulmonary hemorrhage or bronchial exsanguination.
What is Hemoptysis?
Hemoptysis is characterized by the vomiting of blood originating from the lungs or bronchi as a result of pulmonary hemorrhage or bronchial exsanguination.
- Hemoptysis is classified as nonmassive or enormous based on the volume of blood misfortune; in any case, there are no uniform definitions for these categories
- Hemoptysis is considered nonmassive in case blood misfortune is less than 200 mL per day.
- The lungs get blood from the aspiratory and bronchial blood vessel systems.
- The low-pressure aspiratory framework tends to create small-volume hemoptysis, while dying from the bronchial framework, which is at systemic weight, tends to be profuse.
- Blood misfortune volume is more valuable in coordinating administration than in coming to a determination.
What is the Contrast Between Hacking Up Blood and Spewing Blood?
Hacking up blood (hemoptysis) isn't the same as spewing blood (hematemesis). Blood that's hacked up ordinarily looks like blood-stained spit blended with bodily fluid. Heaving blood includes regurgitating huge amounts of blood. It ordinarily includes inner dying in your upper gastrointestinal (GI) tract.
See a healthcare supplier quickly if you're spewing blood.
Is Hacking Up Blood Genuine?
It can be. It all depends on what's causing your blood misfortune and the degree of your blood misfortune. Most causes aren't genuine and are treatable. Still, hacking up blood can be a sign of genuine conditions, like serious contamination or lung cancer. Losing as well as much blood at once can be life-threatening and require crisis therapeutic consideration.
As it were a healthcare supplier can decide how genuine your condition is. If you're hacking up huge amounts of blood, or in case your condition doesn't progress, see a supplier.
What are the Causes of Hemoptysis?
Hemoptysis can have numerous causes within the human body.
Irresistible causes incorporate: -
- Bronchitis
- Tuberculosis
- Lung sore
- Pneumonia
Non-infectious hemoptysis causes incorporate: -
- Lung cancer
- Generous development within the lungs injury or harm Taking torment solutions without taking after appropriate enlightening
- Unlawful drugs such as cocaine
- Smoking
Within the primary care setting, the foremost common causes of hemoptysis are intense and unremitting bronchitis, pneumonia, tuberculosis, and lung cancer.
- Disease
The disease is the foremost common cause of hemoptysis, bookkeeping for 60 to 70 percent of cases. The disease causes shallow mucosal aggravation and edema that can lead to the burst of the superficial blood vessels. In a review study of inpatient and outpatient hemoptysis within the Joined together States, bronchitis caused 26 percent of cases, pneumonia caused 10 percent, and tuberculosis accounted for 8 percent. Intrusive microbes (e.g., Staphylococcus aureus, Pseudomonas aeruginosa) or parasites (e.g., Aspergillus species) are the foremost common irresistible causes of hemoptysis. Viruses such as the flu too may cause serious hemoptysis. Human immunodeficiency infection (HIV) contamination inclines patients to a few conditions which will deliver hemoptysis, counting pulmonary Kaposi's sarcoma.
Essential lung cancers account for 23 percent of cases of hemoptysis within the Joined together States. Bronchogenic carcinoma may be a common lung cancer mindful of hemoptysis in 5 to 44 percent of all cases. Dying from dangerous or kind tumors can be auxiliary to shallow mucosal attack, the disintegration into blood vessels, or exceedingly vascular injuries. Breast, renal, and colon cancers incline lung metastasis; be that as it may, metastatic lung carcinoma occasionally comes about in bleeding. Obstructive injuries may cause an auxiliary disease, coming about in hemoptysis.
- Pneumonic venous hypertension
Cardiovascular conditions that result in aspiratory venous hypertension can cause cardiac hemoptysis. The foremost common of these is clearing out ventricular systolic heart disappointment. Other cardiovascular causes incorporate extreme mitral stenosis and pulmonary embolism. Although hemoptysis could be a recognized pneumonic embolism indication, pneumonic embolism is an exceptional cause of hemoptysis. For illustration, in a quiet without underlying cardiopulmonary illness, the positive and negative probability proportions for hemoptysis in pneumonic embolism are 1.6 and 0.95, separately. Subsequently, the nearness or nonattendance of hemoptysis alone has no critical impact on the likelihood of pulmonary embolism.
- Idiopathy
Idiopathic hemoptysis could be a conclusion of exclusion.
Guess for idiopathic hemoptysis ordinarily is sweet, and the lion's share of patients have the determination of dying within six months of evaluation. Be that as it may, comes about from one study found an expanding frequency of lung cancer in smokers more seasoned than 40 years with idiopathic hemoptysis, and suggested that these patients may warrant near monitoring.
- Hemoptysis in children
The moment the most common cause is outside body yearning, with most cases happening in children more youthful than four long times. Another vital cause is bronchiectasis, which regularly is auxiliary to cystic fibrosis. Essential aspiratory tuberculosis could be an uncommon cause evaluated to happen in less than 1 percent of cases. Although the exceptional, injury is another conceivable cause. Blunt-force injury may result in hemoptysis auxiliary to pulmonary wound and hemorrhage. Dying caused by suffocation, consider or inadvertent, moreover ought to be considered.
Side Effects and Signs of Hyperventilation Disorder
- Intense hyperventilation disorder
Patients with intense hyperventilation disorder display dyspnea in some cases so extreme that they compare it to suffocation. It is gone with by disturbance and a sense of fear or by side effects of chest torment, paresthesias (fringe and perioral), fringe tetany (eg, firmness of fingers or arms), and presyncope or syncope or now and then by a combination of all of these discoveries. Tetany happens since respiratory alkalosis causes both hypophosphatemia and hypocalcemia. On examination, patients may show up on edge, tachypneic, or both; lung examination is unremarkable.
- Persistent hyperventilation disorder
Patients with persistent hyperventilation disorder show distance less significantly and regularly elude discovery; they murmur profoundly and as often as possible and regularly have nonspecific substantial side effects within the setting of temperament and uneasiness clutter and enthusiastic stretch.
Pathophysiology of Hemoptysis
Most of the lung's blood circulates through low-pressure aspiratory supply courses and closes inside the pneumonic capillary bed, where gas is exchanged. Approximately 5% of the blood supply circulates through high-pressure bronchial supply routes, which start at the aorta and supply major aviation routes and supporting structures. In hemoptysis, the blood, by and large, emerges from this bronchial circulation, but when pneumonic courses are harmed by injury, by the disintegration of a granulomatous or calcified lymph hub or tumor, or, seldom, by aspiratory blood vessel catheterization or when pneumonic capillaries are influenced by aggravation.
Diagnosis of Hemoptysis
- History
History of display sickness ought to cover the term and worldly designs (eg, unexpected onset, recurrent repeat), inciting components (eg, allergen introduction, cold, effort, recumbent position), and surmised volume of hemoptysis (eg, streaking, teaspoon, container). Patients may require particular inciting to distinguish between genuine hemoptysis, pseudo hemoptysis (ie, dying originating within the nasopharynx that's in this way hacked up), and hematemesis. A sensation of postnasal trickle or any dying from the nares without hacking is suggestive of pseudo hemoptysis. Concomitant queasiness and heaving with dark, brown, or coffee-ground–coloured blood is characteristic of hematemesis. Foamy sputum, shinning ruddy blood, and (if gigantic) a sensation of choking are characteristics of genuine hemoptysis.
The survey of frameworks ought to look for indications recommending conceivable causes, counting fever and sputum generation (pneumonia); night sweats, weight misfortune, and weakness (cancer, TB); chest torment and dyspnea (pneumonia, pneumonic embolism); leg torment and leg swelling (aspiratory embolism); hematuria (Goodpasture disorder); and wicked nasal release (granulomatosis with polyangiitis).
Patients ought to be inquired almost hazard variables for causes. These hazard components incorporate HIV contamination, utilization of immunosuppressants (TB, contagious contamination); presentation to TB; long smoking history (cancer); and later immobilization or surgery, known cancer, earlier or family history of clotting, pregnancy, utilization of estrogen-containing drugs, and later long-distance travel (aspiratory embolism).
Past restorative history ought to cover known conditions that can cause hemoptysis, counting incessant lung infection (eg, COPD [unremitting obstructive aspiratory infection], bronchiectasis, TB, cystic fibrosis), cancer, bleeding clutters, heart disappointment, thoracic aortic aneurysm, and pulmonary-renal syndromes (eg, Goodpasture syndrome, granulomatosis with polyangiitis). Introduction to TB is vital, especially in patients with HIV disease or another immunocompromised state.
A history of visit nosebleeds, simple bruising, or liver illness recommends conceivable coagulopathy. The medication profile ought to be surveyed for utilize of anticoagulants and antiplatelet drugs.
- Physical Examination
Noteworthy clues frequently will limit the differential conclusion and help centre the physical examination. Looking at the expectoration may offer assistance localize the source of bleeding. The doctor ought to record crucial signs, counting beat oximetry levels, to archive fever, tachycardia, tachypnea, weight changes, and hypoxia. Protected signs such as cachexia and level of quiet trouble too ought to be famous. The skin and mucous layers ought to be reviewed for cyanosis, paleness, ecchymoses, telangiectasia, gingivitis, or proof of dying from the verbal or nasal mucosa.
The examination for lymph hub broadening ought to incorporate the neck, supraclavicular locale, and axillae. The cardiovascular examination incorporates an assessment for jugular venous distention, irregular heart sounds, and edema. The doctor ought to check the chest and lungs for signs of union, wheezing, rales, and injury. The stomach examination ought to center on signs of hepatic clogs or masses, with an assessment of the limits for signs of edema, cyanosis, or clubbing.
- Demonstrative Assessment
Fiberoptic bronchoscopy is favored in case neoplasia is suspected; it is demonstrative for central endobronchial illness and permits coordinated visualization of the dying location. It too licenses tissue biopsy, bronchial lavage, or brushings for pathologic conclusion. Fiberoptic bronchoscopy moreover can give coordinated treatment in cases of proceeded death. Unbending bronchoscopy is the favored apparatus for cases of gigantic dying since of its more noteworthy suctioning and aviation route support capabilities.
High-resolution CT has gotten to be progressively valuable within the beginning assessment of hemoptysis and is favored if the parenchymal infection is suspected. Its complementary utilization with bronchoscopy gives a more prominent positive surrender of pathology and is valuable for barring harm in high-risk patients. Its part in hemoptysis proceeds to advance, and further studies are required to assess its impact on quiet administration and results. Patients with repetitive or unexplained hemoptysis may require extra research facility assessment to set up a conclusion.
Treatment for the Hemoptysis
- Nonmassive hemoptysis
The general objectives of administration of the understanding with hemoptysis are triple: dying cessation, yearning avoidance, and treatment of the fundamental cause. As with any possibly genuine condition, assessment of the “ABCs” (i.e., aviation route, breathing, and circulation) is the beginning step.
The foremost common introduction is intense, gentle hemoptysis caused by bronchitis. Low-risk patients with ordinary chest radiographs can be treated on an outpatient premise with near checking and fitting verbal anti-microbials, in case clinically shown. In case hemoptysis endures or remains unexplained, an outpatient assessment by a pulmonologist ought to be considered.
An anomalous mass on a chest radiograph warrants an outpatient bronchoscopic examination. For patients with a typical chest radiograph and chance components for lung cancer or repetitive hemoptysis, outpatient fiberoptic bronchoscopy moreover is shown to run the show out a neoplasm. High-resolution CT is shown when clinical doubt for danger exists, and sputum and bronchoscopy don't surrender any pathology. High-resolution CT moreover is shown when chest radiography uncovers fringe or other parenchymal infection.
- Enormous hemoptysis
The mortality rate from enormous hemoptysis depends on the death rate and etiology. Hemoptysis more noteworthy than 1,000 mL per 24 hours within the nearness of harm carries a mortality rate of 80 percent30; hence, enormous hemoptysis warrants a more forceful, practical approach. These patients require serious care and early discussion with a pulmonologist. In cases of gigantic or life-threatening hemoptysis, determination and therapy must happen at the same time. Aviation route upkeep is imperative since the essential instrument of passing is suffocation, not exsanguination. Supplemental oxygen and liquid revival are basic. Help from a cardiothoracic specialist ought to be considered since crisis surgical mediation may be required.
It's imperative to note that hemoptysis can be a side effect of a genuine condition, such as lung cancer or pneumonic embolism, so it ought to not be overlooked. If you involve in hacking up blood, look for restorative consideration instantly.









