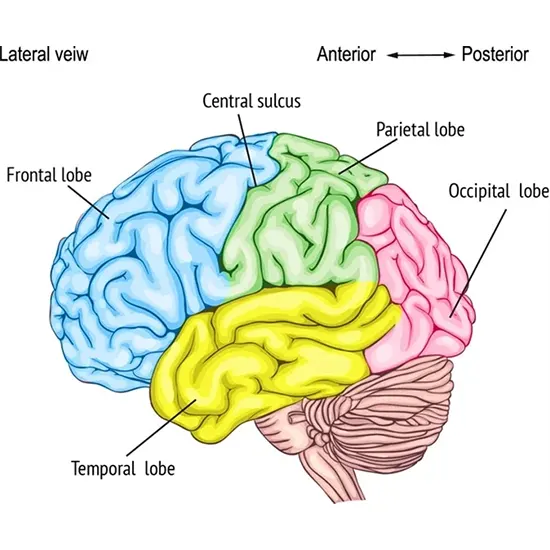
One of the four main lobes of the human brain is the frontal lobe which is situated at the front of the cerebral cortex. It plays a crucial role in many higher-order cognitive functions, such as attention, decision-making,...
Overview
One of the four main lobes of the human brain is the frontal lobe which is situated at the front of the cerebral cortex. It plays a crucial role in many higher-order cognitive functions, such as attention, decision-making, planning, problem-solving, working memory, and social behavior.
The frontal lobe is furthermore responsible for the control of voluntary movement and is involved in regulating emotions and impulse control. Since it is the last portion of the brain to fully mature and is therefore particularly vulnerable to damage from injury or disease.
The frontal lobe can be branched out into various regions, each of which has specific functions.
- The prefrontal cortex is the anterior part and is responsible for functions, such as decision-making and impulse control.
- The motor cortex is the tail portion of the frontal lobe, which controls voluntary movement.
Frontal syndromes, also known as frontal lobe disorders, are a group of neurological conditions that result from damage to the frontal lobes of the brain. These syndromes can have a significant impact on a person's ability to think, reason, and behave appropriately. The severity and nature of the symptoms depend on the extent and location of the damage.
There are several different frontal syndromes, each with its own set of symptoms. Some of the most common frontal syndromes include:
- Frontal lobe dementia
- Frontal lobe epilepsy
- Frontal lobe injury
- Frontotemporal dementia.
- Frontal lobe stroke
This article will give in-depth knowledge of all the frontal syndromes, including their main causes, symptoms, and treatment plan.
"Remembering who you are, every step of the way" - Navigating through frontal dementia
Introduction
Frontal lobe dementia, also known as frontotemporal dementia, is a type of dementia that primarily affects the frontal lobes of the brain. It is an occasional kind, that typically affects individuals under the age of 65, and is often misdiagnosed as Alzheimer's disease.
Signs and symptoms
Some of the signs and symptoms of frontal lobe dementia include:
- Changes in behavior: The individual may exhibit socially inappropriate behavior, lack of empathy, and decreased inhibition.
- Changes in personality: The individual may exhibit a lack of interest in activities they previously appreciated and may become more passive or apathetic.
- Language difficulties: The individual may have trouble finding the right words or understanding language.
- Executive dysfunction: The individual may have difficulty with decision-making, problem-solving, and planning.
- Movement disorders: In some cases, individuals with frontal lobe dementia may develop movement disorders, such as tremors or rigidity.
- Impaired memory: While memory impairment is not a primary symptom of frontal lobe dementia, some individuals may experience difficulty with recall or memory retention.
- Loss of insight: The individual may not recognize their changes in behavior or cognitive abilities.
"Seizing control of epilepsy"- going through frontal epilepsy-
Introduction
Frontal lobe epilepsy is a type of epilepsy that arises in the frontal lobes of the brain. The frontal lobes are liable for a variety of functions, including motor control, decision-making, and social behavior. When seizures occur in the frontal lobes, they can influence these processes and cause a spectrum of manifestations.
Frontal lobe epilepsy is a somewhat rare form of epilepsy, accounting for approximately 7-8% of cases
Signs and Symptoms
The manifestations of frontal lobe epilepsy can vary relying on the area of the frontal lobes affected by the seizures. Some common symptoms of frontal lobe epilepsy include:
- Abnormal movements: The individual may exhibit abnormal movements, such as jerking or twitching of one side of the body or face.
- Changes in behavior: The individual may exhibit changes in behavior or emotion during a seizure, such as fear, panic, or agitation.
- Speech disturbances: The individual may experience difficulty speaking or produce incomprehensible speech during a seizure.
- Confusion or memory loss: The individual may experience confusion or memory loss following a seizure.
- Sensory changes: The individual may experience sensory changes, such as tingling or numbness, during a seizure.
- Lack of awareness: In some cases, the individual may lose consciousness during a seizure.
- Aura: Some individuals with frontal lobe epilepsy may experience an aura, or a warning sensation, at before the onset of a seizure.
Understanding Frontal Injuries-
Introduction
A frontal lobe injury affects the front part of the brain, specifically the frontal lobes.
Signs And Symptoms
Symptoms of a frontal lobe injury can vary relying on the rigor and area of the injury, but may include:
- Changes in personality: The individual may exhibit changes in personality, including increased irritability, impulsivity, and decreased empathy.
- Cognitive deficits: The individual may experience deficits in cognitive function, including memory, attention, and problem-solving abilities.
- Motor deficits: The individual may experience motor deficits, including deficiency or immobility on one side of the body, the problem with coordination or balance, or spasticity.
- Difficulty with language: The individual may experience difficulty with language, including understanding speech or producing speech.
- Emotional changes: The individual may exhibit emotional changes, including depression, anxiety, or apathy.
- Changes in social behavior: The individual may exhibit changes in social behavior, including difficulty with social interactions, decreased social awareness, or inappropriate behavior.
Steering through Frontotemporal dementia
Introduction
Frontotemporal dementia (FTD), also called frontotemporal regression, is a kind that particularly involves the frontal and temporal lobes of the brain. It is a relatively infrequent form of dementia, accounting for approximately 10% of all cases.
FTD typically affects individuals under the age of 65 and can progress rapidly, with a duration of 2 to 10 years
Signs and symptoms
Symptoms of FTD vary depending on the FTD and the individual, but may include:
- Changes in behavior: The individual may exhibit socially inappropriate behavior, lack of empathy, and decreased inhibition.
- Changes in personality: The individual may exhibit an absence of encouragement and may become more passive or apathetic.
- Language difficulties: The individual may have trouble finding the right words or understanding language and may exhibit speech abnormalities.
- Executive dysfunction: The individual may have difficulty with decision-making, problem-solving, and planning.
- Movement disorders: In some cases, individuals with FTD may develop movement disorders, such as tremors or rigidity.
- Impaired memory: While memory impairment is not a primary symptom of FTD, some individuals may have trouble with recall or memory retention.
- Loss of insight: The individual may not recognize their own changes in behavior or cognitive abilities.
"Stroke can occur to anyone, at any point of time." Knowing Frontal Stroke
Introduction
A frontal lobe stroke is a type of stroke that happens when the frontal lobe's blood supply of the brain is interrupted, causing a loss of function. The frontal lobes are accountable for a variety of functions, including motor control, decision-making, and social behavior.
Signs and symptoms
The symptoms of a frontal lobe stroke may vary depending on the location and severity of the stroke but may include:
- Difficulty with movement or coordination: The individual may experience difficulty with balance, coordination, or walking.
- Changes in behavior: The individual may exhibit changes in behavior, including decreased inhibition, impulsivity, or apathy.
- Difficulty with decision-making or problem-solving: The individual may have difficulty making decisions or solving problems.
- Language difficulties: The individual may have trouble finding the right words or understanding language.
- Emotional changes: The individual may exhibit emotional changes, including depression, anxiety, or apathy.
- Changes in social behavior: The individual may exhibit changes in social behavior, including difficulty with social interactions, decreased social awareness, or inappropriate behavior.
"Don't guess, test "- Diagnostic tests for frontal syndromes.
There are diverse tests that can be utilized to consider these conditions, including clinical, radiographic, and laboratory tests.
Clinical Tests:
- Neuropsychological testing: This test assesses a person's cognitive abilities, including memory, attention, language, and problem-solving skills.
- Clinical examination: This involves a physical exam and evaluation of the patient's neurological function, including reflexes, muscle strength, coordination, and balance.
- Psychiatric evaluation: This can help to identify any underlying mental fitness issues that may be pitching into the patient's symptoms.
Radiographic Tests:
- MRI (Magnetic Resonance Imaging): This technique employs the usage of magnetic fields and radio waves to develop thorough images of the brain. Structural abnormalities in the frontal lobes, such as tumors or lesions can be specified.
- CT (Computed Tomography): This imaging technique uses X-rays to create thorough images of the brain. It can help to identify structural abnormalities, such as hemorrhages, edema, or atrophy.
Laboratory Tests:
- Blood tests: These can be used to determine any cardinal medical ailments that may be contributing to the patient's symptoms, such as thyroid dysfunction or vitamin deficiencies.
- CSF (Cerebrospinal fluid) analysis: This involves analyzing a specimen of the fluid that envelops the spinal cord and brain. It can help to determine illnesses or inflammation in the brain.
Overall, the diagnosis of frontal syndromes requires a comprehensive evaluation that includes a combination of clinical, radiographic, and laboratory tests. The particular tests used may differ relying on the individual patient's symptoms and medical history.
Comprehensive Treatment Approach to fight frontal syndromes-
Treatment choices for frontal syndromes depend on the underlying cause of the condition and may include medication, surgery, or a combination of both.
Medication:
- Antidepressants: Frontal syndromes often involve changes in mood and behavior, and antidepressant medications such as selective serotonin reuptake inhibitors (SSRIs) can help relieve signs of depression and apprehension.
- Antipsychotics: These medications can be helpful in managing delusions, hallucinations, and other symptoms of psychosis that may be associated with frontal syndromes.
- Mood stabilizers: For individuals with mood swings or bipolar disorder, mood stabilizing medications such as lithium may be beneficial in controlling symptoms.
- Stimulants: Medications such as methylphenidate or amphetamines may be helpful in improving focus and reducing impulsivity in people with attention deficit hyperactivity disorder (ADHD) or other disorders associated with inattention or impulsivity,
Surgery:
In a few special cases, surgical intervention may be necessary for the treatment of frontal syndromes. A handful of the surgical options available are:
- Deep brain stimulation: This involves implanting electrodes in specific areas of the brain and stimulating those areas with electrical impulses to enhance function and reduce symptoms.
- Lesionectomy: This involves the removal of a selected area of the brain that is causing symptoms, such as a tumor or lesion.
- Lobectomy: This pertains to the reduction of a portion of the frontal lobe in cases where seizures are the first symptom.
- Hemispherectomy: In severe cases where the frontal syndrome is caused by a severe brain injury or malformation, a hemispherectomy could also be necessary. This affects the deduction of 1 half of the brain.
It is significant means that these treatments are highly specialized and should only be considered after a radical evaluation by a professional neurologist or neurosurgeon.
"Managing the multifaceted impacts"- Complications of Frontal Syndromes.
Frontal Syndromes can lead to a range of complications that can impact different aspects of a person's life. Some of the common complications of Frontal Syndromes include:
Behavioral problems: Frontal Syndromes can cause a person to experience behavioral changes such as impulsivity, apathy, disinhibition, and aggression.
Cognitive impairment: Individuals with Frontal Syndromes may experience difficulties with memory, attention, problem-solving, and decision-making.
Emotional instability: Frontal Syndromes can lead to emotional instability, including mood swings, depression, anxiety, and social withdrawal.
Speech and language impairment: Damage to the frontal lobe can result in speech and language difficulties such as aphasia, a disorder that deforms a person's capacity to express.
Motor deficits: Individuals with Frontal Syndromes may experience difficulties with movement and coordination, including muscle weakness, tremors, and difficulties with balance.
Impaired social and interpersonal skills: Individuals with Frontal Syndromes may have difficulties with social interactions, which can lead to problems with relationships, employment, and other aspects of daily life.
Increased risk-taking behavior: Individuals with Frontal Syndromes may be more prone to engage in risky behaviors, which can lead to casualties.
Reduced insight into their condition: Individuals with Frontal Syndromes may have a reduced awareness of their condition, which can make it challenging to seek and receive appropriate medical care.









