One kind of brain tumour is an astrocytoma. They begin in a specific subtype of glial cells, the astrocytes, which are star-shaped brain cells located in the cerebral cortex. Typically, this form of tumour does not affect...
One kind of brain tumour is an astrocytoma. They begin in a specific subtype of glial cells, the astrocytes, which are star-shaped brain cells located in the cerebral cortex. Typically, this form of tumour does not affect other organs or spread outside of the brain and spinal cord. Astrocytomas are the second most frequent type of glioma after glioblastomas and can develop in almost all areas of the brain, as well as the spinal cord on occasion.
Two major categories of astrocytomas are recognised in the literature, including those:
Narrow zones of infiltration are frequently well-defined on diagnostic images and are primarily non-invasive tumors, such as pilocytic astrocytomas, subependymal giant cell astrocytomas, and pleomorphic xanthoastrocytoma.
Diffuse zones of infiltration, such as high-grade astrocytomas, have a propensity for the cerebral hemispheres but can develop in any part of the central nervous system. They typically affect adults and have an innate tendency to advance to more advanced grades.
Astrocytomas can occur in people of any age. Children and young adults are more likely to have the low-grade kind than adults are, whereas adults are more likely to have the high-grade kind. Approximately 75% of neuroepithelial tumors are astrocytomas, which are more prevalent in young people.
Pathophysiology
By compressing, invading, and destroying brain parenchyma, causing arterial and venous hypoxia, competing for nutrients, releasing metabolic waste products (such as free radicals, altered electrolytes, and neurotransmitters), and releasing and attracting cellular mediators (such as cytokines), an astrocytoma disrupts normal parenchymal function and has regional effects. Elevated intracranial pressure brought on by a direct mass effect, a rise in blood volume, or a rise in cerebrospinal fluid volume might result in secondary clinical consequences.
Hereditary and atomic modifications
Homozygous cancellation of CDKN2A and CDKN2B is the highlight of tall-review astrocytoma. In addition, a genome-wide design of DNA copy-number changes (CNAs) has been revealed, which is related to a patient's survival and reaction to treatment. This design distinguishes among lower-grade astrocytoma patients a subtype where the CNA genotype is highly related to a one-year survival phenotype.
Classification
Astrocytomas may be cancerous or noncancerous. The World Health Organisation (WHO) categorizes astrocytomas into four grades. The grades depend on how quickly astrocytomas develop and the probability that they'll spread to and penetrate adjacent brain tissue. Grade 1 astrocytomas are the mildest, whereas grade 4 astrocytomas are the most forceful.
Noncancerous astrocytomas
Grade 1 astrocytoma, which is noncancerous, and includes:
Pilocytic astrocytoma:
This is often a slow-growing tumor that doesn't tend to spread. It's the most common type of astrocytoma. It's kind and doesn't require chemotherapy or radiation treatment after it's surgically evacuated. Pilocytic aftercare Thomas more cells are regularly created in your cerebellum.
Pleomorphic xanthoastrocytoma:
This tumor often develops gradually and most frequently creates in your worldly projection. It frequently causes seizures. Surgery, as a rule, cures this sort of brain tumor.
Subependymal monster cell astrocytoma (SEGA):
This tumor primarily occurs in children who have tuberous sclerosis, a hereditary condition. It develops interior ventricles, which are fluid-filled spaces deep in your brain. Surgery, as a rule, cures it.
Cancerous astrocytomas incorporate:
Grade 2 astrocytomas:
These astrocytomas tend to spread to adjacent brain tissue. Due to this, surgery alone might not be sufficient to treat them.
Grade 3 astrocytomas:
These astrocytomas are more forceful than grade 2 astrocytomas and frequently show movement compared to grade 2 astrocytomas. Surgery alone never cures these tumors. They require radiation and almost always require chemotherapy.
Glioblastomas:
These are grade of four astrocytomas. They're the most common type of astrocytoma and the most forceful; they develop and spread quickly. They can either display as a cancerous movement from an already existing lower-grade astrocytoma (10% of cases) or start as a grade 4 tumor (90% of cases).
Indications
Glioma indications depend on the area of the glioma. Side effects, meanwhile, may depend on the type of glioma, its estimate, and how rapidly it's developing.
Common signs and symptoms of gliomas include:
- Cerebral pain, especially one that is most prevalent in the morning,
- Sickness and heaving
- perplexity or decay in brain work, such as issues with considering and understanding data.
- Memory misfortune.
- Identity changes or crabbiness
- vision issues, such as obscured vision, twofold vision, or the misfortune of fringe vision.
- Discourse challenges.
- Seizures, particularly in somebody who hasn't had seizures recently.
Causes
- Specialists aren't sure what causes glioma. It begins when cells within the brain or spinal cord create changes in their DNA. A cell's DNA contains the instructions that tell the cell what to do.
- The DNA changes tell the cells to create more cells rapidly. This causes numerous other cells to not work right. The cells form a mass called a tumor.
- The tumor can develop to press on adjacent nerves and parts of the brain or spinal cord. This leads to glioma indications and can cause complications.
- A few gliomas create more changes in their DNA that cause them to end up with brain cancers. The changes tell the cells to attack and annihilate healthy brain tissue.
- In gliomas, the tumor cells are compared to normal brain cells called glial cells. The glial cells encompass the back nerve cells within the brain and spinal cord.
- Radiation presentation and astrocytomas
- Exposure to ionizing radiation, such as from radiation treatment, increases your risk of developing an astrocytoma.
For example, children who get prophylactic (preventive) radiation for intense lymphocytic leukaemia are 22 times more likely to create a central apprehensive framework tumor, such as astrocytoma, within about five to 10 years.
Hereditary qualities and astrocytomas
The development of rare genetic conditions is associated with the advancement of astrocytomas.
Li-Fraumeni disorder:
This condition happens when something changes in your TP53 quality. Individuals who have Li-Fraumeni disorder have a 90% chance of developing one or more types of cancer in their lifetimes, which may include astrocytoma.
Neurofibromatosis type 1 (NF1):
This condition causes irregular increments in cell development due to a transformation in a quality that's gathered to smother tumor development. Individuals with NF1 can develop early-onset astrocytomas, fringe nerve tumors, and spots on their skin called café-au-lait spots.
Tuberous sclerosis:
This condition causes an assortment of therapeutic issues, counting epilepsy, formative delay, and tumors throughout your body.
Tuberous sclerosis is caused by changes in two qualities:
TSC1 and TSC2 Subependymal mammoth cell astrocytomas (SEGAs) are ordinarily found in, as it were, Caucasian individuals with tuberous sclerosis.
Turcot disorder:
This condition comes about when there are transformations in a few qualities that stifle tumor development. Turcot disorder frequently includes developments (polyps) in your intestinal tract and one or more brain or spinal-line tumors, such as an astrocytoma.
Risk components
Things that can increase the hazard of glioma include:
Getting older: Gliomas are most common in adults between the ages of 45 and 65. But gliomas can happen at any age. Certain sorts of gliomas are more common in children and young adults.
Being uncovered to radiation: Individuals who have been exposed to a sort of radiation called ionizing radiation have an expanded chance of developing glioma. One application of ionizing radiation is the radiation treatment used to treat cancer.
Having a family history of glioma: Gliomas can run in families, but this can be exceptionally uncommon. More inquiries are required to get it, and parents can pass on a hazard of glioma to their children.
Who does astrocytoma influence?
Astrocytomas can influence anybody, but diverse grades tend to influence individuals of diverse ages:
Grade 1: Astrocytomas mostly frequently influence children and high schoolers.
Astrocytomas, Grade the 2 most frequently influencing adults between 20 and 60.
Astrocytomas (Grade 3), which most often affect grownups between 30 and 60,
Glioblastoma (Grade 4 astrocytomas) most frequently affects adults between 50 and 80.
Grade 3 and 4 astrocytomas are more likely to influence grown-ups assigned male at birth than adults assigned female at birth.
How common is astrocytoma?
Different grades of astrocytoma are more common than others:
Review 1: Astrocytomas account for 2% of all brain tumors.
Review 2 Astrocytomas account for 2%–5% of all brain tumors.
Review 3 Astrocytomas account for 4% of all brain tumors.
Review 4 Astrocytomas (glioblastomas) account for 24% of brain tumors.
In adults, glioblastoma (review 4 astrocytomas) is the most common sort of brain cancer.
Conclusion
Tests and procedures used to analyse astrocytomas incorporate:
Neurological exam. During a neurological exam, your specialist will tell you about your signs and symptoms. He or she may check your vision, hearing, coordination, quality, and reflexes. Issues in one or more of these zones may give clues to almost the entire portion of your brain that may be influenced by a brain tumor.
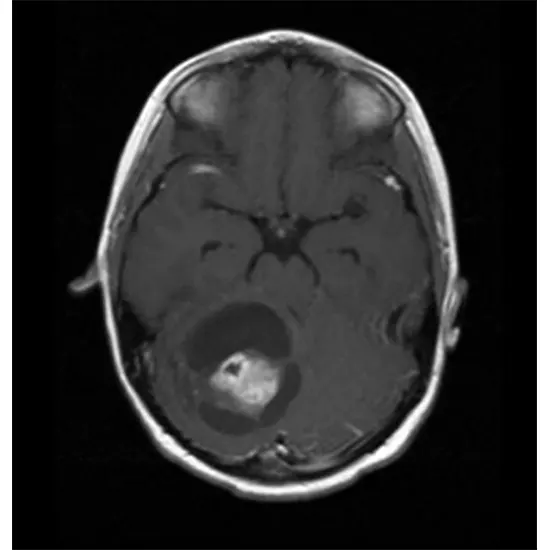
Imaging tests. Imaging tests can assist to your specialist in determining the area and size of your brain tumor. MRI is frequently used to diagnose brain tumors, and it may be used alongside specialized MRI imaging techniques, such as useful MRI, perfusion MRI, and attractive reverberation spectroscopy.
Other imaging tests may incorporate CT and positron emission tomography (PET).
Expelling a sample of tissue for testing (biopsy) A biopsy can be done with a needle during recent surgery or after surgery to evacuate your astrocytoma, depending on your specific circumstances and the area of your tumor. The test of the suspicious tissue is analysed in a research facility to determine the sorts of cells and their level of forcefulness.
Specialized tests of the tumor cells can tell your specialist what types of mutations the cells have obtained. This gives your specialist clues almost your guess and may direct your treatment alternatives.
Treatment
Astrocytoma treatments incorporate:
Surgery
Surgery to evacuate the astrocytoma Your brain specialist (neurosurgeon) will work to expel as much of the astrocytoma as is conceivable. The objective is to evacuate all of the cancer, but some of the astrocytomas were found to be delicate organs or tissues, which were also hazardous. Indeed, evacuating a few cancers may diminish your signs and indications.
For some people, surgery may be the treatment needed. For others, additional treatments may be recommended to kill any cancer cells that might stay and decrease the risk that cancer will return.
Radiation treatment
Radiation treatment employs high-energy bars, such as X-rays or protons, to slaughter cancer cells. Amid radiation treatment, you lie on a table while a machine moves around you, coordinating pillars with specific points in your brain.
Radiation treatment may well be prescribed after surgery on the off chance that your cancer wasn't expelled or on the off chance that there's an expanded risk that your cancer will return. Radiation is frequently combined with chemotherapy for aggressive cancers. For individuals who can't experience surgery, radiation treatment and chemotherapy may be utilized as essential treatments.
Chemotherapy
Chemotherapy uses drugs to murder cancer cells. Chemotherapy drugs can be taken in pill form or through a vein in your arm. In certain circumstances, a circular wafer of chemotherapy medication can be placed in your brain after surgery, where it gradually breaks up and discharges the medication.
Chemotherapy is often utilized after surgery to kill any cancer cells that might remain. It can be combined with radiation treatment for aggressive cancers.
Clinical trials
Clinical trials are thought of as new treatments. These things give you a chance to undertake the most recent treatment options, but the chance of side effects may not be known. Inquire with your doctor whether you can be qualified to take part in a clinical trial.
supportive (palliative) care. Palliative care is specialized restorative care that focuses on providing relief from torment and other indications of a genuine illness. Palliative care professionals work with you, your family, and your other specialists to provide an additional layer of support that complements your continuous care. Palliative care can be used while experiencing other forceful medicines, such as surgery, chemotherapy, or radiation treatment.
Adjuvant treatments for astrocytomas
Adjuvant treatment, sometimes called "partner treatment," targets cancer cells that primary treatment didn't crush. In the case of astrocytomas, surgery is the essential treatment.
Review 3 and review 4 astrocytomas continuously require medications other than surgery alone. Review 2: Astrocytomas may sometimes require adjuvant treatment.
Adjuvant treatments for astrocytomas incorporate:
Chemotherapy with temozolomide (TMZ):
Chemotherapy involves solutions that crush cancer cells and/or prevent them from duplicating. Temozolomide (TMZ) is a sedate that works by changing the DNA of tumor cells and, in this way, causing the cells to pass on. TMZ is a first-line adjuvant treatment for each of reviews 3 and reviews 4 astrocytomas. Suppliers now and then endorse it for review 2 astrocytomas.
Radiation treatment:
This treatment employs radiation (as a rule, high-powered X-rays) to kill cancer cells. It's ordinarily exceptionally effective in making a difference in treating astrocytomas.
Bevacizumab:
Usually, an infused medicine anticipates blood vessels from making a difference in tumor-level development. U.S. Nourishment and Sedate Organisation (FDA) have approved bevacizumab for repetitive glioblastomas. It helps reduce swelling and can assist in moving forward with side effects.
Tumor-treating areas:
Typically, uncommon gadgets produce electrical areas that can delay tumor growth. You wear it like a protective cap. Healthcare suppliers may prescribe this treatment for recently analyzed and repetitive glioblastomas.
What is the prognosis of astrocytoma?
The forecast (viewpoint) of astrocytoma depends on a few variables, including:
Tumor grade:
The guesses, by and large, get more regrettable as the review progresses.
How much of the tumor can be surgically removed?
Whereas grade 1 astrocytomas are usually cured with surgery alone, it's incomprehensible to completely remove grade 2 through 4 astrocytomas. In any case, the more tissue the neurosurgeon can remove, the better the survival rate.
Utilise adjuvant treatment:
Adjuvant treatments, such as chemotherapy and radiation treatment, can offer assistance in minimizing indications and increasing the survival rate.
Age:
In general, youth is related to longer survival.
Mental status:
Minimal side effects and typical neurological work are related to longer survival.









