BPH, also known as benign prostatic hyperplasia, is a disease in which men's prostate glands enlarge but are not cancerous. Additional phrases for benign prostatic hyperplasia comprise benign prostatic obstruction and...
What is benign prostatic hyperplasia?
BPH, also known as benign prostatic hyperplasia, is a disease in which men's prostate glands enlarge but are not cancerous. Additional phrases for benign prostatic hyperplasia comprise benign prostatic obstruction and benign prostatic enlargement.
As male ages, the prostate experiences two major growth phases. The prostate increases in size during the first phase of puberty. Around the age of 25, the second stage of growth starts, and it lasts for most of the man's existence. The second growth period frequently coincides with benign prostatic hyperplasia.
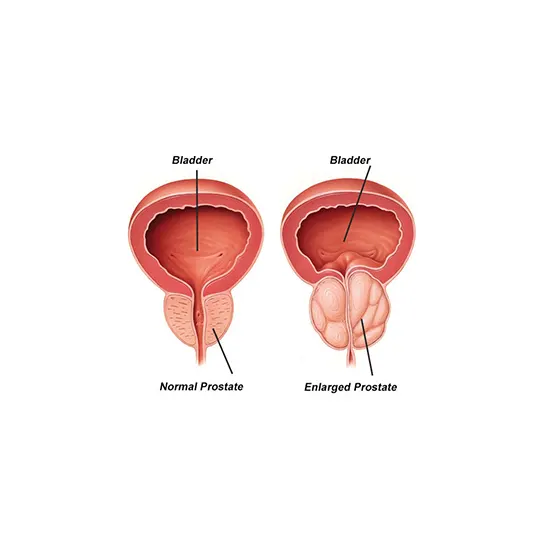
The urethra is lifted and squeezed against the prostate as it rises in size. A thickening of the bladder membrane occurs. The bladder may eventually deteriorate and lose its capacity to clear entirely, leaving some urine in the bladder.
Prostate
Part of the male reproductive system is the prostate, a walnut-shaped organ. Making a substance that transforms into semen is the prostate's primary job. A man's ability to reproduce depends on his prostate secretions. The urethra is encircled by the gland at the bladder's throat. The ureter and bladder are connected at the bladder neck. A portion of the lower urinary system is the bladder and urethra. The prostate is discovered just below the bladder, in front of the rectum, and has two or additional lobes, or parts, that are surrounded by an outer layer of tissue. The tube that extends from the bladder to the outside of the body to excrete pee is known as the urethra. Men's urethras also discharge semen through them.
What causes benign prostatic hyperplasia?
Benign prostatic hyperplasia primarily affects older males, but its exact cause is unknown. Men with removed testicles before puberty do not acquire benign prostatic hyperplasia. For this reason, some experts think that aging and testicular factors may contribute to benign prostatic hyperplasia.
Men make small amounts of estrogen, a female hormone, and testosterone, a male hormone, throughout their lives. Men's blood levels of active testosterone decline with age, leaving a larger percentage of estrogen. According to scientific research, benign prostatic hyperplasia may happen because the prostate's estrogen content stimulates the activity of molecules that encourage prostate cell growth.
Dihydrotestosterone (DHT), a male hormone that influences the growth and expansion of the prostate, is the subject of one more hypothesis. According to some studies, older men continue to produce and accumulate high amounts of DHT in the prostate despite a decline in blood testosterone levels. The build-up of DHT may promote the growth of prostate cells. Men who do not generate DHT do not experience benign prostatic hyperplasia, according to scientists.
How common is bph?
For men over 50, prostate problems are prevalent. Up to 14 million American males had lower urinary tract symptoms that could have been caused by benign prostatic hyperplasia in 2010.1 even though benign prostatic hyperplasia rarely manifests indications before the age of 40, incidence and signs rise with age. About 50% of men between the ages of 51 and 60 and up to 90% of men over the age of 80 retain benign prostatic hypertrophy.
Groups affected:
Benign prostatic hyperplasia in men is more prone to occur in those with the following conditions:
- Age 40 and later
- Benign prostatic hyperplasia in the family,
- Obesity
- Heart and circulatory disease
- Type 2 diabetes
- Inactivity
- Erectile dysfunction
Symptoms
Indications of benign prostatic hyperplasia in the lower urinary system include.
- urine frequency: eight or more daily urination
- Urinary urgency, also known as an unwillingness, to postpone urination, difficulty initiating a urine stream, a weak or interrupted urine stream, or dribbling urine after urination
- nocturia, or frequent urination and urine retention while sleeping.
- urinary incontinence—accidental loss of pee—pain following ejaculation or during urination, abnormally coloured urine, or abnormal odor
Most of the time, benign prostatic hyperplasia symptoms are.
- A ureter obstruction
- A strained bladder from attempting to move urine through the obstruction.
The degree of the obstruction or the symptoms is not always correlated with prostate growth. While some men with significantly enlarged prostates experience little blockage and few symptoms, other men with minimally enlarged prostates experience more symptoms and a higher degree of blockage. Less than half of men with benign prostatic hyperplasia experience symptoms in their lower urinary system.
Men occasionally don't become aware of a blockage until they are unable to pee. Taking over-the-counter cold or allergy medicines that contain decongestants, such as pseudoephedrine and oxymetazoline, can cause this condition, known as acute urinary retention. These drugs may have a side effect that staves off the bladder and neck from unwinding and releasing urine. Antihistamine-containing medications, such as diphenhydramine, can impair bladder muscle contraction, which results in urinary retention, trouble urinating, and painful urination. Urinary retention in males with partial urethra blockage can also be brought on by booze, cold weather, or extended periods of inactivity.
Complications
Benign prostatic hyperplasia problems could include the following:
- A severe accumulation of urine
- Urinary tract infections and long-lasting or persistent urinary retention with blood in the pee (UTIs)
- Pelvic injury
- Renal injury
- Urethral stones
The majority of males with benign prostatic hyperplasia do not experience these side effects. However, when it happens, kidney damage can pose a significant health risk.
When to go see your doctor?
A person may encounter urinary signs that are detached from benign prostatic hyperplasia and are carried on by bladder issues, urinary tract infections, or prostatitis—prostate inflammation. Benign prostatic hyperplasia symptoms can also be a sign of more severe conditions, such as prostate cancer.
Men with benign prostatic hyperplasia signs ought to see a doctor.
Men with the following signs and symptoms need to see a doctor right away:
- absence of any capacity to urinate.
- Urination is painful, frequent, and urgent, and there is blood in the urine and severe discomfort or pain in the lower abdomen and urinary system.
Diagnosis
A medical professional makes the diagnosis of benign prostatic hypertrophy using.
- medicine background, both personal and family
- medical analyses and a physical analysis
Personal and family medical history
Taking a personal and family medical history is one of the first things a healthcare provider may do to help diagnose benign prostatic hyperplasia. A healthcare provider may ask a man.
- What Signs Are Present
- When The Symptoms Began and How Frequently They Occur
- Whether He Has a History Of Recurrent UTIs
- What Medicines He Takes, Both Prescription and Over the Counter
- How Much Fluid He Typically Consumes Each Day
- Whether He Consumes Caffeine and Alcohol
- About His General Medical History, Including Any Significant Illnesses or Surgeries
Physical examination
Benign prostatic hyperplasia may be identified through a medical examination. A medical professional typically performs a thorough examination during a:
- Checks a patient's body, which may include looking for enlarged or tender lymph nodes in the groin or discharge from the urethra.
- A patient's swollen or painful scrotum presses on particular part of their body.
- Conducts a manual rectal examination.
A physical examination of the prostate is performed during a digital rectal evaluation. The doctor instructs the patient to lie on his side or lean over a table while holding his knees close to his chest to conduct the examination.
Medical examination
However, the health care practitioner most frequently diagnosed benign prostatic hyperplasia established on symptoms and a digital rectal exam. Men may be referred to a urologist, a physician who specializes in urinary issues and the male reproductive system. A urologist can identify and prescribe treatment for lower urinary tract issues caused by benign prostatic hyperplasia using medical tests. medical exams could consist of
- Prostate-specific Antigen in Urine (Psa) Examination of Blood
- Urinalysis Exams
- Cystoscopy
- Ultrasonography Transrectal Biopsy
Urinalysis
A pee sample is examined during a urine analysis. In a medical professional's workplace or another setting, the patient collects a urine sample in a special container. The sample is examined by a doctor during an office appointment or sent to a lab for examination. A nurse or technician administers the test by dipping a dipstick—a piece of chemically treated paper—into the urine. When there are indications of infection in the urine, patches on the dipstick change color.
PSA blood test
During an office appointment or in a commercial setting, a healthcare professional can take blood for a PSA test and send the sample to a lab for evaluation. PSA is a peptide that is produced by prostate cells. PSA grades in men with prostate cancer may be boosted more than normal. However, prostate cancer is not always indicated by a high PSA reading. Elevated PSA levels are frequently brought on by benign prostatic hyperplasia, prostate infections, inflammation, aging, and regular fluctuations. There is still much to learn about how to interpret a PSA blood test, how well it can distinguish between cancer and benign prostate conditions like benign prostatic hyperplasia, and what to do if the PSA number is high.
Urodynamic tests
Numerous methods are used in urodynamic tests to assess how effectively the bladder and urethra store and release urine. Urodynamic tests are carried out by a healthcare professional in a hospital, outpatient facility, or during an office appointment.
Some urodynamic studies can be performed without anesthesia, while others might need local anesthesia. Most urodynamic tests, which may include the following, concentrate on the bladder's capacity to store urine and empty consistently and fully:
Reduced urine flow or residual urine in the bladder, which frequently indicates urinary blockage brought on by benign prostatic hyperplasia, is measured by uroflowmetry, which gauges how quickly the bladder releases urine, and post-void residual measurement.
Cystoscopy
During a cystoscopy technique, the urethra and bladder are visualized inside a tube-like device named a cystoscope. The lower urinary system is entered by a urologist using the cystoscope through the opening at the tip of the penis. A urologist can conduct a cystoscopy in a hospital, outpatient facility, or during an office visit. The patient will receive local anesthesia from the doctor, but occasionally the patient may also need sedation and regional or general anesthesia. Using a cystoscopy, a urologist can check the urinary system for obstructions or stones.
Transrectal ultrasound
A transducer is a tool that safely and painlessly bounces sound waves off organs to produce an image of their anatomy during the transrectal ultrasound. To check various organs, the medical professional can position the transducer at various angles. The process is carried out by a specially trained technician in a doctor's office, an outpatient facility, or a hospital; there is no need for the patient to be sedated. A radiologist, a physician who specializes in medical imaging, interprets the images. Transrectal ultrasound is the method that urologists use the most to check the prostate. A detector about the length of a pen is inserted into the man's rectum, right next to the prostate, during a transrectal ultrasound. The size of the prostate abnormalities is visible on the ultrasound picture.
Biopsy
A small piece of prostate tissue is removed during a biopsy process to be examined under a microscope. The biopsy is carried out by a urologist in a hospital or an ambulatory facility. The patient will receive a local anesthetic and mild sedation from the urologist; however, in some circumstances, the patient will also need general anesthesia. The biopsy probe is guided into the prostate by the urologist using imaging methods like ultrasound, computerized tomography, or magnetic resonance imaging. The prostate tissue is analysed in a facility by a pathologist, a medical specialist who concentrates on analysing tissues to identify diseases. The examination can indicate the existence or absence of prostate cancer.
Treatment
Treatment for benign prostatic hyperplasia depends on the patient's preferences, the severity of the symptoms, and how much they interfere with his daily living.
Men with a mildly enlarged prostate may not require therapy unless their symptoms are visible and hurt their quality of life. In these situations, a urologist might advise routine checks in place of medical intervention. A urologist will typically advise therapy if benign prostatic hyperplasia symptoms become bothersome or pose a health risk.









