The belly and retroperitoneum are both susceptible to abscesses. They mostly happen following operations, injuries, or illnesses that cause irritation and infection in the abdomen, especially when peritonitis or perforation...
The Issue's Description
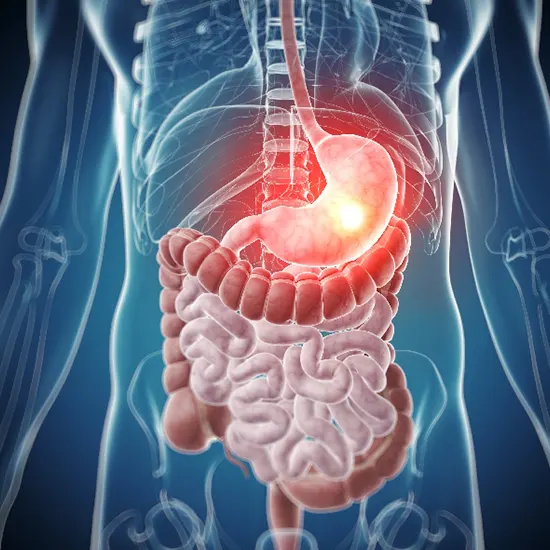
The belly and retroperitoneum are both susceptible to abscesses. They mostly happen following operations, injuries, or illnesses that cause irritation and infection in the abdomen, especially when peritonitis or perforation take place. Abscess discomfort, fever, and malaise are symptoms. CT is used to diagnose. Surgical or percutaneous draining is the mode of treatment. Antibiotics are optional.
An abdominal infection is what?
An abscess is a pus-filled area of inflamed tissue. Anywhere on the body, abscesses can develop. (both inside and outside). The surface of the skin is where they are most frequently located.
A pus-filled space in the belly is known as an abdominal abscess.
Abdominal abscesses can develop around organs in the abdomen, such as the liver, pancreas, and kidneys, or close to the interior of the abdominal wall, at the rear of the abdomen, or in these locations. Although abdominal abscesses can appear for no obvious reason, they are typically connected to other incidents like intra-abdominal surgery, bowel ruptures, or abdominal injuries.
Intra-Abdominal Abscesses' Etiology
Intraperitoneal, retroperitoneal, and ventral intra-abdominal abscesses are the three categories. Following colon cancer or the rupture of a hollow viscus, many intra-abdominal abscesses form. Others arise from the spread of an infection or an inflammatory response to illnesses like appendicitis, diverticulitis, Crohn's disease, pancreatitis, pelvic inflammatory disease, or really any illness that results in generalised peritonitis. Another important risk factor is abdominal surgery, especially when it involves the gastrointestinal or biliary tract: Anastomotic leaks, for example, can cause the peritoneum to become contaminated during or after operation. Whether or not they are operated on, traumatic abdominal injuries, especially lacerations and hematomas of the liver, pancreas, spleen, and intestines, can lead to the development of abscesses.
A complex mixture of anaerobic and aerobic bacteria make up the infecting organisms, which usually reflect healthy bowel flora. These individuals are most frequently found:
- Breathable gramme-negative bacteria (eg, Escherichia coli and Klebsiella)
- Anaerobes (especially Bacteroides fragilis)
An abdominal infection develops for what reason?
The bacteria that cause abdominal abscesses typically reach the gut as a result of penetrating trauma, bowel rupture, or intra-abdominal surgery. When an organ or the abdominal cavity is compromised in some manner that allows bacteria access, intra-abdominal abscesses (abscesses within the abdomen) can form. These ailments include Crohn's disease and ulcerative colitis, intestine rupture, penetrating injuries, surgery, and appendicitis. There could be additional causes, depending on where the abdominal abscess is.
Additionally, abscesses can develop in the region between the vertebrae and the abdominal cavity. Retroperitoneal abscesses are the name for these lesions. The area between the vertebrae and the abdominal cavity is referred to as the retroperitoneum.
Pathophysiology
Within the peritoneal region, an intra-abdominal abscess can either be localised or widespread. Localized pus accumulation might have an omentum, adhesions, or other nearby viscera as a barrier. Abdominal abscesses typically contain a polymicrobial assemblage of GI tract-derived aerobic and anaerobic organisms. The bacteria typically cause an inflammatory response that frequently leads to a hypertonic environment where an abscess hole continues to grow. An abdominal abscess can cause septic sepsis if it is not addressed.
Endogenous microbes seep into the affected cavity and cause anaerobic infections. The anaerobic organism could be displaced, though, if the host's defence systems are disturbed.
What signs indicate a stomach abscess?
Abdominal abscesses commonly exhibit the following symptoms:
Experiencing abdominal discomfort
Fever, hunger loss, and vomiting
How is an infection in the abdomen identified?
The signs of other, less severe conditions may resemble the signs of an abdominal abscess. To make a precise diagnosis, your doctor might perform an imaging exam. The first testing device that is used might be an ultrasound. Your doctor can also see the organs and cells of the abdomen with the aid of additional imaging tests like a CT scan or an MRI.
Ultrasound
High-frequency sound waves are used in abdominal ultrasounds to produce pictures of the organs in the abdomen.
Your abdomen will be visible as you lay on a table for the exam. A clear, water-based gel will be applied to the skin over the belly by an ultrasound technician. Then they will pass a portable device known as a transducer over the belly. High-frequency sound waves from the transducer are reflected off of internal organs and bodily parts. A computer receives the waves and utilises them to generate images. Your doctor can carefully inspect abdominal organs thanks to the images.
CT image for computerised tomography
A CT scan is a unique type of X-ray that can display cross-sectional images of a particular bodily part.
The gantry, or big circle with a hole in the center, is how the CT scanner appears. You'll lie flat on a table that is placed inside the gantry during the scan. The gantry will then start to revolve around you as it takes multiple images of your abdomen. This provides your doctor with a thorough look of the region.
Organs, localised abscesses, abdominal growths, and foreign items in the body can all be seen on a CT scan.
Magnesium-based imagery (MRI)
To produce images of the body, an MRI employs powerful magnets and radio waves. Long magnetic tubes make up the MRI scanner.
You will be placed on a bed that slips into the test tube's opening. Your body is surrounded by a magnetic field created by the generator, which aligns the water molecules there. This enables the device to take precise cross-sectional pictures of your belly.
Your doctor will find it simpler to examine any anomalies in the tissues and organs of the abdomen with an MRI.
Analysis of an abscess drainage sample
To provide a more accurate diagnosis, your doctor may draw a sample of fluid from the abscess and analyse it. The technique used to collect a fluid sample relies on where the abscess is located.
How is an infection in the abdomen treated?
Important management principles
The level of patient acuity, the speed of the procedure, and the patient's tolerance for any delay in more invasive definitive management (such as percutaneous drainage/decompression or exploratory laparotomy for diagnosis or therapeutic intent) must all be taken into consideration when developing an idealised management plan. In sicker patients, concurrent diagnostic, stabilization, and source management are recommended.
Make the sufferer more stable. Even with ongoing resuscitation, immediate surgical intervention is necessary for diffuse peritonitis and ought to be thought of as a stabilising operation that can be done quickly.
Cognitive recognition
Awareness in the brain (i.e. consider the diagnosis of intra-abdominal infection). This is simpler for isolated instances of typical abdominal symptoms, but more challenging when they are unusual, muted, or nonexistent as a result of altered mental status, analgesic use, corticosteroid use, other immunosuppression, chronic liver disease, or a predominate concurrent extraabdominal condition (respiratory failure, myocardial infarction, stroke, diabetic ketoacidosis). With bladder pressure tracking and either surgical or non-surgical decompression, the diagnosis of abdominal compartment syndrome should be taken into account in patients with tense abdominal distension.
Tests In The Lab That Are Diagnostic
In general, a full blood count, differential, chemical, and blood culture are necessary for every patient. On the basis of pre-test clinical suspicion, some studies are performed. For instance, right upper quadrant pain and other signs of hepatobiliary infection should trigger the measurement of lipase/amylase and liver-associated enzymes. If the patient has ascites that is clinically apparent, a paracentesis should be done with the aid of ultrasound for a cell count, differential, gramme's stain, and culture.
Radiography Diagnostic Tests
Plain abdominal films may show "free air," an abnormal pattern of gas indicative of partial or total obstruction, thickened bowel loops, stones, or vascular calcifications indicative of mesenteric ischemia. The presence of peritonitis, perforated viscous, an intra-abdominal abscess, or an obstructed viscus on an abdominal radiograph may be a normal or non-specific observation. The data obtained from abdominal CT imaging is significantly better and has a greater sensitivity and specificity.
Empiric antibiotic treatment
Three risk factors that should be evaluated to improve the precision of empiric treatment include recent antimicrobial exposure, length of hospital stay of more than 5 days, and illness severity. These risk factors are linked to a high prevalence of multidrug-resistant pathogens. Antimicrobials should then, if at all possible, be restricted after determining conclusive cultures and susceptibilities. The most frequent targets are intestinal facultative gramme negative bacilli, enterococci, and obligate anaerobes. Examples of these include E. coli, Klebsiella, Enterobacter, Serratia, and Proteus. (Bacteroides fragilis and non-fragilis spp., Peptostreptococci, Clostridium spp., Fusobacteria spp.).
For a successful result, the most important intervention. The goal is to handle the source of the infection definitively, which may involve debriding necrotic or devitalized tissue, draining fluid that is infected or contaminated, or draining necrotic or devitalized fluid. Even when other diagnostic and stabilisation procedures are underway, patients with diffuse peritonitis require immediate surgery. In cases where a patient is extremely unstable and unlikely to benefit from surgery or a healing procedure (such as intra-abdominal hypertension), two or more stages of an intervention should be used, with the first stage focusing on harm control and the second on definitive correction.
2. Emergency Preparedness
Keeping the patient steady
If septic manifestations are present, they must be treated quickly and forcefully in order to minimise the risk of subsequent organ failure and prepare the patient for source control procedures.
Transfer to an intensive care unit for patients who are deteriorating quickly and who require adequate nursing care, monitoring, and resuscitation.
placement of arterial line, Foley catheter, and big bore peripheral intravenous catheters (or central venous access). Vomiting, dizziness, and distension may all call for a nasograstric intubation.
Tracking and assistance with hemodynamics
The vast majority of patients who display SIRS, severe sepsis, or shock will need 2-4+ litres of crystalloid fluid support, which is best titrated to urine flow rate, correction of acidosis, heart rate and blood pressure, and central venous pressure higher than 12-15 mm Hg. Pressor support is adjusted to a mean arterial blood pressure range of 60 to 65 mm Hg. The ideal standard is central venous access for both volume and pressor infusion as well as CVP monitoring; however, if central access cannot be rapidly obtained, fluid resuscitation should not be delayed and can be given by large bore peripheral access. Mixed venous saturation of greater than 65%, serum lactate, and correction of base deficit are all acceptable measurable resuscitation goals.
Consultation in interventional or surgical radiography for the implementation of a source control strategy.
One of the initial stages in treating an abdominal abscess is drainage. Pus from an abscess can be removed using needle extraction, among other techniques.
Your doctor will perform this treatment by inserting a needle through your skin and right into the abscess while using a CT scan or ultrasound as guidance. The plunger will then be pulled by your doctor to drain all the liquids. Your doctor will submit a sample to the lab for testing after draining the abscess. This will facilitate choosing the appropriate medicines.
Antibiotics given intravenously will also be necessary to address the abdominal abscess.
Some situations might call for operation. Surgery might be required:
- If an organ has ruptured and the abscess is tough to access with a needle, it should be cleaned out more thoroughly.
- In order to make you unconscious throughout the procedure, your doctor will administer general anaesthesia. The surgeon will make a cut in the abdomen during the operation to find the abscess.
- The abscess will then be cleaned, and a drain will be attached so that pus can flow out. Up until the abscess is healed, the drain will remain in position. Normally, this takes a few days or weeks.
Multiple Diagnoses
- Long-term ileus
- Unknown cause of fever Crohn's illness
- inflammatory colitis
- infected perianal cervix in complexity
- invasive colon carcinoma
- Abscess with diverticulum
Prognosis
Before the advent of the CT scan, the prognosis for people with an abdominal abscess was very good. Since CT scans are now widely available, the diagnosis is made much sooner, and in many cases, CT-guided drainage has reduced morbidity. However, the mortality rate is very high if an abdominal abscess is misidentified and left untreated. The following risk variables can lead to an increase in mortality and morbidity:
- maturity in advance
- Multiple organ failure
- multiple previous operations
- advanced cyst
- protracted prognosis
Complications
These problems could result from an abdominal abscess:
- Multiple organ failure
- development of a fistula
- Stomach distress
- Bowel perforation can result from surgery as well as CT-guided evacuation.
- Death
- Malnutrition Deep venous thrombosis
Care following surgery and rehabilitation
Typically, patients with abdominal abscesses need to remain in the hospital. In order to confirm that there are no remaining abscesses after therapy, repeat imaging is frequently performed.
Some people might need total parenteral nutrition depending on how complicated the abscess is.
Physical therapy is advised because the patients are frequently elderly in order to regain flexibility and muscle power.
Conclusion
Hollow viscous organs and solid organs are the two primary sites where intra-abdominal abscesses develop. The development of an abscess can result from hollow-organ perforation caused by luminal obstruction, inflammation, trauma, and anastomotic disturbance. Solid-organ abscesses can be caused by hematogenous infections, infection in continuity, and bacterial incursion. The majority of severe intra-abdominal infections are discovered after surgery, but laparotomies rarely result in an infection.
Pain, tachycardia, and fever are common complaints, but other symptoms, like anorexia and weight loss, may not be as particular. Fluid shifts that can be fatal as well as systemic inflammatory reaction syndrome can be brought on by severe infections. The source and severity of the infection are evaluated using laboratory and imaging tests.
Treatment success depends on the use of cardiorespiratory support, antibiotic medication, and source control measures (like percutaneous or surgical drainage). Malnutrition, advanced age, severe underlying illness, and ineffective antimicrobial therapy are risk factors for increased mortality from intra-abdominal infections.









