Red blood cells contain a protein namely Hemoglobin and it carries oxygen throughout the body. A disorder in which there is abnormal production of hemoglobin is referred to as Thalassemia syndrome. People who suffer from...
What Can Be Epidemiology?
The epidemiology of thalassemia varies by region, with the highest prevalence found in the Mediterranean region, Middle East, South Asia, and Southeast Asia.
The exact prevalence of thalassemia is difficult to determine due to the different nature of the disease and the lack of standard methods of diagnosis. However, it is estimated that thalassemia affects around 5% of the global population, with approximately 270 million carriers and 300,000-500,000 affected individuals.
The distribution of thalassemia varies by ethnicity, with higher prevalence rates found in certain ethnic groups. For example, beta thalassemia is most commonly found in individuals of Mediterranean, Middle Eastern, and South Asian descent, while alpha thalassemia is more common in individuals of African and Southeast Asian descent.
The prevalence of thalassemia also varies by subtype and severity. Beta thalassemia major is the largely brutal form of the disease and is relatively rare, with an estimated incidence of 1 in 100,000 live births. Beta thalassemia minor is more common, with an estimated carrier frequency of 1-5% in some populations. Alpha thalassemia can also range from mild to severe, with the most severe form (hemoglobin Bart's hydrops fetalis syndrome) occurring almost exclusively in Southeast Asia.
In recent years, advances in genetic testing and counseling have helped to reduce the incidence of thalassemia in some populations. However, the disease remains an important public health situation in numerous portions of the world, particularly in low- and middle-income countries where access to healthcare and genetic testing is limited.
Knowing The Pathogenesis of This Condition.
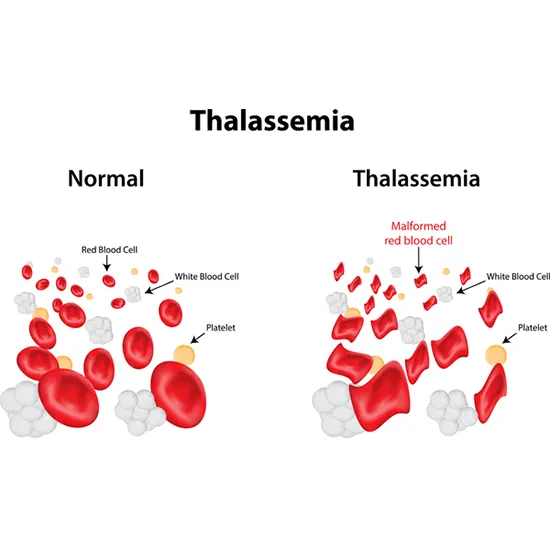
Thalassemia syndrome is a group of inherited blood disorders characterized by fewer or missing production of one or more of the globin chains that make up hemoglobin, the protein responsible for carrying oxygen in the blood.
The pathogenesis of thalassemia involves a complex interplay of genetic, molecular, and cellular events. This infection is a consequence of transformations in the genes that code for the alpha or beta globin chains. These mutations lead to an imbalance in the synthesis of the globin chains, resulting in reduced production of the affected chain and an excess of the unaffected chain.
The pathogenesis of thalassemia also involves a range of cellular and molecular mechanisms. In both types of thalassemia, the imbalance in the synthesis of the globin chains leads to a build-up of unpaired globin chains, which can form toxic aggregates and cause damage to the red blood cells. This can lead to hemolysis (the destruction of red blood cells), anemia (a decrease in the number of red blood cells), and a range of clinical manifestations associated with reduced oxygen delivery to the tissues.
In addition, the excess of unpaired globin chains can activate a range of cellular stress pathways, leading to oxidative stress, inflammation, and cellular damage. This can further exacerbate the symptoms of thalassemia and contribute to the development of complications such as iron overload, endocrine abnormalities, and increased susceptibility to infections.
What Are Different Forms of This Syndrome?
Two different types of thalassemia include alpha thalassemia and beta thalassemia.
1. Alpha Thalassemia: Alpha thalassemia is caused by mutations in the genes that produce alpha globin, a protein that forms part of hemoglobin. There are four genes involved in producing alpha globin, and the severity of alpha thalassemia depends on how many of these genes are affected. Four types of alpha thalassemia include:
- Silent Carrier: One of the four alpha globin genes is missing or non-functional. People with this type of alpha thalassemia have no symptoms and carry this disorder.
- Alpha Thalassemia Trait: Two of the four alpha globin genes are missing or non-functional. People with this type of alpha thalassemia may have mild anemia but usually have no other symptoms.
- Hemoglobin H Disease: Three of the four alpha globin genes are missing or non-functional. People with this type of alpha thalassemia have moderate to severe anemia and may experience fatigue, weakness, and other symptoms.
- Hydrops fetalis: All four alpha globin genes are missing or non-functional. This is the most severe form of alpha thalassemia and is usually deadly before or momentarily after delivery.
2. Beta Thalassemia: Beta thalassemia is caused by mutations in the genes that produce beta-globin, a protein that forms part of hemoglobin. Two different types of beta thalassemia include:
- Beta Thalassemia Minor: People with this type of beta thalassemia have one normal beta globin gene and one mutated beta globin gene. They may have mild anemia but usually have no other symptoms.
- Beta Thalassemia Major: People with this type of beta thalassemia have two mutated beta globin genes. This is a greatly harsh form of beta-thalassemia and causes severe anemia, bone deformities, organ damage, and other complications. Treatment for beta thalassemia major usually involves regular blood transfusions and other supportive care.
What Can Be The Causes?
Hemoglobin is made up of two types of protein chains, alpha, and beta globin. In thalassemia, there are mutations in the genes that produce either the alpha or beta globin chains, leading to a deficiency or absence of one or both types of chains.
In alpha thalassemia, four genes produce alpha globin proteins. If one or more of these genes are mutated, it can lead to a deficiency in alpha globin and cause alpha thalassemia. The harshness of alpha thalassemia counts on the number of genes that are affected.
In beta thalassemia, two genes produce beta globin proteins. If one or both genes are mutated, it can lead to a deficiency in beta-globin and cause bet-thalassemia. The severity of beta thalassemia also depends on the number of genes that are affected and the specific mutation.
Thalassemia is an inherited disorder, which means that it is passed down from parents to their children. People with a family history of thalassemia are in a raised danger of creating the disorder. Thalassemia is more common in people of Mediterranean, Middle Eastern, and Southeast Asian descent.
In some cases, thalassemia can also be caused by a de novo mutation, which means that the mutation occurred spontaneously in the dramatic person and was not inherited from either parent.
Let's Talk About Different Signs and Symptoms.
Common signs and symptoms of thalassemia include:
- Anemia: Thalassemia can cause anemia, which is a condition in which there is a depletion of red blood cells or hemoglobin in the blood. Anemia can induce exhaustion, deficiency, and shortness of breath.
- Pale skin: People with thalassemia may have pale or yellowish skin, which is a sign of anemia.
- Slow growth: Children with thalassemia may have slow growth and delayed puberty due to the effects of anemia on the body.
- Abnormal bone growth: Thalassemia can cause abnormal bone growth, which can lead to deformities and other skeletal abnormalities.
- Enlarged spleen: Thalassemia can cause the spleen to enlarge, which is further responsible for pain and discomfort in the abdomen.
- Jaundice: Thalassemia can cause jaundice (yellowing of the skin).
- Heart problems: Thalassemia can cause heart problems, including an enlarged heart and arrhythmias (irregular heartbeats).
- Iron overload: Thalassemia can cause iron overload in the body, which can damage organs such as the liver, heart, and pancreas.
- Frequent infections: People with thalassemia may be more susceptible to infections due to the effects of anemia on the immune system.
Don't Wait to Get Diagnosed Today.
Different diagnostic options include:
- Blood tests: A complete blood count (CBC) can reveal low levels of hemoglobin and red blood cells, which are common in people with thalassemia. Additional blood tests may be performed to measure the levels of other blood components, such as iron and ferritin.
- Hemoglobin electrophoresis: This is a laboratory technique used to separate the different types of hemoglobin in a blood sample. Thalassemia can be identified by the presence of abnormal hemoglobin variants or imbalances between different types of hemoglobin.
- DNA analysis: Genetic testing can be used to identify specific mutations in the alpha or beta globin genes that cause thalassemia. DNA analysis can also help determine the carrier status of individuals who may be at risk of passing on thalassemia to their children.
- Prenatal testing: If a parent is a known carrier of thalassemia, prenatal testing can be performed to determine if the fetus has inherited the disorder. This can be done using chorionic villus sampling (CVS) or amniocentesis.
- Newborn screening: Some states require new-borns to be screened for thalassemia as part of routine newborn screening. This involves a blood test that looks for abnormal levels of hemoglobin or other blood components.
Together We Can Overcome This - Treatment.
Depending on the severity of the condition, treatment for thalassemia may involve regular blood transfusions, medication, and/or bone marrow transplantation.
- Blood transfusions: People with thalassemia major, the most severe form of the condition, require regular blood transfusions to replace the abnormal hemoglobin in their red blood cells with healthy hemoglobin. The frequency of transfusions varies depending on the severity of the thalassemia and can range from once every few weeks to once every few months.
- Iron chelation therapy: Frequent blood transfusions can cause iron overload, which can damage organs like the liver, heart, and endocrine glands. To prevent this, iron chelation therapy is used to remove excess iron from the body. This can be done through medications like deferoxamine or deferasirox, which bind to iron in the blood and allow it to be excreted.
- Folic acid supplementation: People with thalassemia have an increased rate of red blood cell destruction, which can lead to a deficiency of folic acid. Supplementation with folic acid can help to prevent complications like anemia and fatigue.
- Bone marrow transplantation: In severe cases of thalassemia, bone marrow transplantation may be a treatment option. This involves replacing the patient's bone marrow, which produces abnormal red blood cells, with healthy bone marrow from a donor.
The Prognosis May Be Uncertain, But the Fight Is Not Over - Prognosis.
People with thalassemia major have a poor prognosis without treatment.
The prognosis for people with thalassemia intermedia is generally better than for those with thalassemia major, but it still depends on the severity of the individual's condition and how well it is managed.
Thalassemia minor, the mildest form of the condition, usually doesn't require treatment and has no significant impact on life expectancy. However, people with thalassemia minor may experience mild anemia or other symptoms.
Overall, the prognosis for thalassemia has improved significantly with advances in medical treatments, such as blood transfusions, chelation therapy, and bone marrow transplantation. People with thalassemia who receive appropriate treatment and care can expect to live relatively normal and healthy lives.
What If Left Untreated?
Depending on the severity of the condition, people with thalassemia can have various complications such as:
- Anemia: Thalassemia causes anemia, which means there are not adequately wholesome red blood cells to carry oxygen to the body's tissues. Anemia can cause fatigue, weakness, shortness of breath, and other symptoms.
- Iron overload: People with thalassemia who receive regular blood transfusions can develop iron overload, which occurs when the body absorbs too much iron from the transfused blood. Iron overload can cause organ damage, particularly to the liver, heart, and endocrine glands.
- Infections: People with thalassemia are at increased risk of infections, particularly those caused by bacteria that normally live in the gut. This is because the body's immune system is weakened by anemia and other factors associated with thalassemia.
- Bone problems: Thalassemia can cause bone problems, such as osteoporosis or bone deformities, particularly in the face and skull.
- Enlarged spleen: Thalassemia can cause the spleen to enlarge, which further causes abdominal pain and discomfort.
- Cardiovascular disease: Thalassemia can increase the risk of cardiovascular diseases, such as heart attacks and stroke.
- Delayed growth and development: Children with severe thalassemia may experience delayed growth and development due to chronic anemia and other factors.









