Inflammatory cells infiltrate various layers of the cornea in keratitis as a result of unpleasant stimuli, such as infectious foreign pathogens or self-antigens. Ulcers may develop as a result of the corneal stroma and...
Inflammatory cells infiltrate various layers of the cornea in keratitis as a result of unpleasant stimuli, such as infectious foreign pathogens or self-antigens. Ulcers may develop as a result of the corneal stroma and epithelium melting suppuratively as a result of the inflammatory response. As a result, the integrity of the globe is threatened in addition to the loss of corneal clarity.
In such circumstances, corneal blindness may occur. Based on clinical characteristics and relevant diagnostic procedures, this activity assists medical professionals in determining the etiological agent as soon as possible and managing these patients with the most recent therapy options.
Keratitis is an inflammation of the cornea that is characterised by ciliary congestion, inflammatory cell infiltration, and corneal edoema. It is linked to both infectious and non-infectious conditions that can affect the entire body or only the surface of the eye.
Among the keratitis kinds mentioned above, "microbial keratitis" makes up the majority and is largely a source of serious worry in underdeveloped nations. Noninfectious keratitis, especially in wealthy countries, cannot be mocked.
Our first line of defence is powerful enough to knock off most infections that cause harm, but some organisms can get past it and spread infection. Such a barrier is the corneal epithelium. In the absence of cellular injury, the majority of the organisms cannot cause keratitis because Giemsa Stain they cannot enter healthy epithelium. The pathogenic organisms that have the ability to penetrate even intact epithelium and produce keratitis include Neisseria meningitides, Neisseria gonorrhoea, Corynebacterium diphtheria, Haemophilus influenza, and Listeria species.
Etiology
Keratitis can be categorised as follows depending on the etiological agent:
Keratitis infectious:
- Pseudomonas, Staphylococcus, Streptococcus, Moraxella, Nocardia, and Atypical Mycobacteria are only a few examples of bacteria that can cause keratitis.
- Protozoal keratitis include Acanthamoeba Keratitis and Pythium Keratitis from oomycete. Although they resemble fungi morphologically, this species' cell wall includes (1-3)(1-6) beta D glucan[2], unlike fungi.[3]
- Aspergillum, Fusarium, Candida (yeast), Cladosporium, Alternaria, Curvularia, and Microsporidia are among the fungi that can cause fungal keratitis.
- Herpes simplex virus (HSV), Herpes zoster virus (HZV), adenovirus, and other viruses can also cause viral keratitis.
- Onchocercal keratitis (sclerosing keratitis) caused by helminths.
Keratitis without infection:
- Among the local causes include trichiasis, large papillae, and a foreign body in the sulcus subtarsalis.
- Keratitis periphery with ulcers
- Rheumatoid arthritis, systemic lupus erythematosus, granulomatosis with polyangiitis, polyarteritis nodose, recurrent polychondritis, and others are collagen vascular disorders.
- Trigeminal nerve injury after surgery or a tumour causes neurotrophic corneal ulcers (post-herpetic zoster ophthalmicus).
- Xerophthalmia
Epidemiology
The incidence of ulcerative keratitis was reported to be 27.6/100000 person-years in a California epidemiological investigation.Contact lens wearers had a considerably greater incidence of ulcerative keratitis.
According to a study done in South India, middle-aged men had a higher risk of developing corneal ulcers than women did.Due to their line of work, farmers face tremendous danger. In poor countries, Gram Stain fungal corneal ulcers are extremely prevalent. HSV remains a significant issue in wealthy countries, nevertheless. Epithelial disease incidence was 15.6/100000 person-years in a Rochester, Minnesota epidemiological research, while stromal keratitis incidence was 2.6/100000 person-years.
Accounts for an estimated 3 per million annual occurrence.
In a research conducted in rural Ethiopia, the prevalence of xerophthalmia was close to 21% and was mostly related to other signs of generalised malnutrition.The majority of the population at risk for xerophthalmia are young children who are undernourished.
Pathophysiology
Corneal Ulcer Stages:
- Progressing penetration stage
- Active ulceration stage
- Regression stage
- cicatrisation stage
Keratitis infectious
The recruitment of macrophages and polymorphonuclear leukocytes is stimulated by infection. The hydrolyses and proteases that these inflammatory cells release are mostly to blame for the stromal melt and necrosis of Acid Fast Bacilli Stain the cornea. Endotoxin has a significant function in gram-negative infections and contributes to the inflammatory response further.
Keratoconjunctivitis caused by a virus
- Stage 1 is characterised by diffuse punctate epithelial keratitis and lasts for 7 to 10 days.
- Stage 2: Sub-epithelial to anterior stromal infiltrates occur after 7 days. The first to act and further involve cell-mediated immunity are NK cells.
- Stage 3 is distinguished by sub-epithelial to anterior stromal infiltrates that persist.
Keratitis Resulting from Onchocerca Volvulus
However, as they pass away after chemotherapy or spontaneously, motile worm infections of the cornea do not directly result in blindness; instead, they produce inflammation and corneal punctate opacification. Blindness can develop from repeated events that cause the cornea to become completely opaque.
Keratitis Ulcerate Periphery
Although the exact cause is unclear, humoral and cell-mediated immunity both play crucial roles. The immunological complex is deposited in the peripheral cornea in response to a corneal antigen. Another mechanism mentioned is the hypersensitive reaction to an exogenous antigens.
Xerophthalmia
For the preservation and integrity of the epithelial lining of the ocular surface, vitamin A deficiency is required. Keratomalacia is caused by the loss of the epithelial lining of the cornea, which is followed by liquefactive necrosis.
Histopathology
Ulcerations of the epithelium frequently precede corneal infections. The breakdown of Bowman's layer and subsequent stromal necrosis occur as a result of polymorphonuclear (PMN) and lymphomononuclear cell infiltration into the stroma. Descent’s membrane perforation is a B Scan ultrasound possibility in serious instances. Suppurative infections result in stromal infiltrates in the anterior two thirds and abscess formation. With persistent infections, it is possible to experience epithelial regeneration, vascularisation, edoema, giant cell reaction, myofibroblastic transformation, stromal remodelling (scarring), and round cell infiltration.
Evaluation
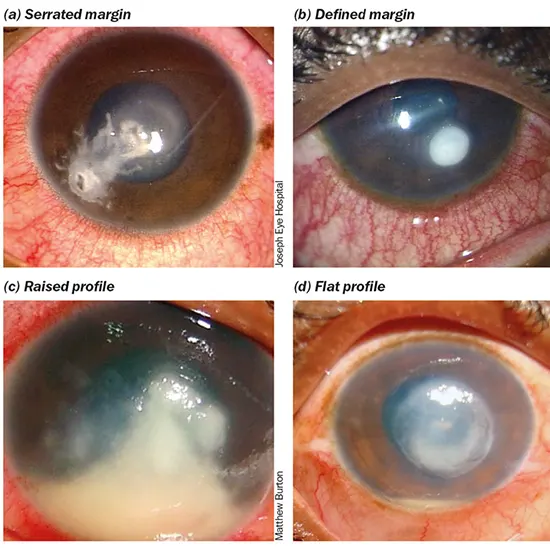
To rule out clogged nasolacrimal duct produced keratitis in all corneal ulcer patients, regurgitation on pressure over the lacrimal sac area (ROPLAS) and/or sac syringing represent critical regular investigations. Any corneal ulcer should be treated according to the standard protocol, which includes looking for the ulcer's distinctive characteristics and then scraping the cornea to find the organism that caused it. Sensitive slides and culture are sent with the sample. Two slides are typically produced, one for Gramme staining and the other for 10% KOH mounting.
Direct microscopy results are used to initiate the patient's drug regimen; afterwards, the treatment plan is adjusted in response to culture results. For the growth of microorganisms, blood and chocolate agar are often used culture medium. For fungi, dextrose agar and potato dextrose agar are used, and non-nutrient agar with E. coli is utilised for Acanthamoeba.
Treatment
Patients with bacterial keratitis are empirically treated on fortified topical antibiotics until culture reports are available. Both gram-positive and gram-negative pathogens are completely covered by fortified cefazolin 5%, vancomycin, fluoroquinolone, tobramycin, or gentamicin. Topical vancomycin is the recommended treatment for keratitis brought on by methicillin-resistant Staphylococcus aureus (MRSA).MRSA can also be treated with 0.2% topical linezolid.
Based on the history and clinical symptoms, a doctor must have a high degree of suspicion to diagnose Acanthamoeba keratitis. Prior topical steroid treatment may improve the organism's yield in smears and cultures, but it also lowers the prognosis. Antiviral pre-treatment may change the clinical image since the clinical picture frequently resembles viral keratitis. The cysts appear in Gramme staining as many double-walled cysts with an inner polyhedral lining. Acanthamoeba cysts are also visible when 10% KOH-mount or 10% KOH with 0.1% calcofluor white is used. E. coli-seeded non-nutritional agar is utilised for culture. The two cornerstones of treatment are biguanides and pentamidine.
Prognosis
Generally speaking, corneal ulcers heal more slowly. In comparison to fungal corneal ulcers, bacterial ulcers recover more quickly. Complete recovery from canthamoeba keratitis could take weeks or even months. The most typical consequence after corneal ulcers is corneal scarring. For later management, these situations can be treated with spectacles, optical iridectomy, or optical keratoplasty to restore eyesight. The prognosis is typically poorer for perforated corneal ulcers. The prognosis for fungal and Acanthamoeba keratitis is worsened by prior topical steroid usage.









