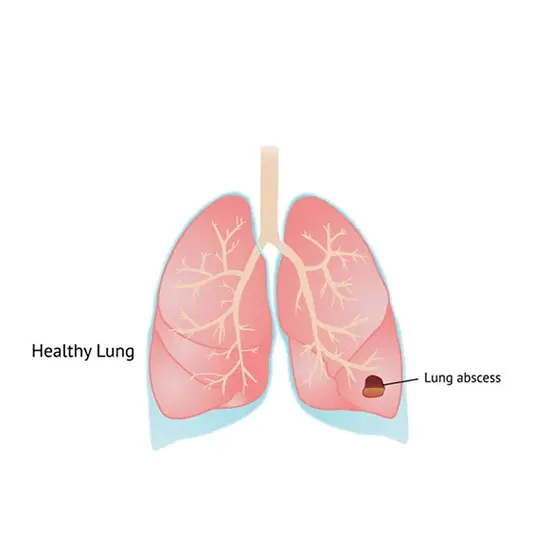
The creation of cavities (more than 2 cm) containing necrotic debris or fluid and liquefaction necrosis of the lung tissue are both symptoms of lung abscess, which are brought on by microbial infection. It can be brought on by...
Abstract
The creation of cavities (more than 2 cm) containing necrotic debris or fluid and liquefaction necrosis of the lung tissue are both symptoms of lung abscess, which are brought on by microbial infection. It can be brought on by aspiration, which can happen when under the influence of drugs or alcohol and typically results in a pus-filled cavity. Moreover, alcohol abuse is the most frequent condition that increases the risk of lung abscesses.
A pulmonary abscess is classified as primary (60%) when it develops from an already present lung parenchymal condition and as secondary (after the rupture of an extrapulmonary abscess into the lung) when it complicates another process, such as vascular emboli.
The substance inside the thorax can be identified using a variety of imaging modalities, including a thoracic CT scan and thoracic ultrasonography. The mainstay of treatment is a broad-spectrum antibiotic to protect against mixed bacteria. Also crucial are postural drainage and pulmonary physiotherapy. In some cases, surgical operations are necessary for pulmonary resection or drainage. We will cover every piece of recent knowledge, from diagnosis to treatment, in this overview.
Discussion
A confined area of pus or necrotic material in the lung parenchyma that leads to a cavity, together with the development of a bronchopulmonary fistula, is referred to as a lung abscess. The liquid content of the cavity.
Or
Lung gangrene and necrotizing pneumonia, both of which are characterised by the presence of many abscesses, are examples of lung infections that also involve lung abscess.
Hippocrates provided the earliest description of the clinical symptoms and treatment for pulmonary abscess. Before the development of antibiotics, lung abscess patients had a one-third mortality rate, a two-thirds full recovery rate, and a remaining three-quarters survival rate with complications such as chronic lung abscess, pleural empyema, or bronchiectasis. At that time, surgery was considered the only effective therapy, and today most patients will be fully recovered only with antibiotic therapy.
Before there were no antibiotics available, a single species of bacteria produced lung abscesses. Today, polymicrobial flora is almost always to blame.
Several Types of Lung Abscesses:
- In terms of duration, there are two categories:
- acute (lasting less than 6 weeks)
- chronic (lasting more than 6 weeks).
Under the Aetiology:
- Primary (necrotizing pneumonia, immunodeficiency, oropharyngeal secretion aspiration);
- Secondary (bronchial obstructions, hemogenic dissemination, direct spread from mediastinal infection, from the supremum, concomitant lung illnesses)
Way of Spreading:
- Bronchogenic
- Haematogenic
Symptoms and Indications
Early Indications of Lung Abscess:
- Which include fever with shaking
- Coughing
- Night sweats
- Diarrhoea
- Weight loss and exhaustion
- Chest pain
- Occasionally anaemia cannot be distinguished from pneumonia.
- Initially, the cough is non-productive, but when the bronchus starts to communicate, the productive cough (vomitus) is the characteristic symptom.
- The cough continues to be productive, and haemoptysis may occasionally follow. Clubbing fingers can develop in patients with persistent abscesses.
Mycosis and tuberculosis are excavated as part of the differential diagnosis, however radiological evidence of gas-liquid level is rarely observed the position of the lesion and the clinical symptoms can help decide whether pneumonic cystic sores, like intrapulmonary, found bronchial growths, sequestration, or auxiliary tainted emphysematous bullae, are available. CT scans or ultrasounds can be used to identify a localized pleural empyema.
Differential Diagnoses Include:
- Excavating squamous cellular or microcellular bronchial cancer
- Excavating tuberculosis
- localized pleural empyema
- Infected emphysematous bullae
- Cavitary pneumoconiosis
- Hiatus hernia
- Pulmonary hematoma
- Cavitary infarcts of the lungs
- Wegener's granulomatosis
Distinguishing an abscess from an empyema is a crucial initial step in the evaluation of a lung abscess, even if an empyema can develop as a consequence of an abscess. On imaging, an empyema is found in the pleural space, whereas a lung abscess is shown as a spherical hollow inside the lungs (outside lungs or between lungs and chest wall).
The diagnostic bronchoscopy is a step in the diagnostic process that collects samples for microbiological analysis and confirms the intrabronchial origin of an abscess, tumour, or foreign substance. Sputum examination helps detect microbes or confirm the presence of bronchial cancer.
Risk Factor
Secretions From the Oropharynx Being Aspirated:
- Dental/periodontal infections
- Paranasal sinusitis
- Altered states of consciousness
- Swell disorder
- Gastroesophageal reflux illness
- Frequent vomiting, intubated patients
- Tracheostomy patients
- Nervous recurring paralysis
- Alcoholism
Among the Causes of Haematogenic Spread:
- Abdominal sepsis
- Infectious endocarditis
- Intravenous drug usage
- Infected central venous catheters
- Septic thromboembolisms
Lung Conditions That Coexist:
- Bronchiectasis
- Cystic fibrosis
- Bullous emphysema
- Congenital malformations (pulmonary sequestration)
- Vasculitis, cystitis
- Infected pulmonary infarcts
- Pulmonary contusion
- Broncho-oesophageal fistula
Acute lung abscesses are typically surrounded by a vaguely defined lung parenchyma and a dense layer of necrotic debris. Histologically, the centre of the abscess contains necrotic tissue mixed with bacteria and necrotic granulocytes. There are protected neutrophilic granulocytes, enlarged veins, and fiery oedema nearby.
Persistent lung abscesses typically have an uneven star-like form, a distinct border around the lung parenchyma, and are filled with thick debris or a greyish line. Pus with or without bacteria is found in the abscess's centre. White blood cells go through the pyogenic membrane that surrounds the abscess to cause cavitation within the abscess. Histiocytes, plasma cells, and lymphocytes with pyogenic membranes are embedded in connective tissue.
Pathogenesis
It is possible to find polymicrobial bacteria in more than 90% of lung abscess patients. Gram-negative Bacteroides fragilis, Fusobacterium capsulatum, and neuropore, as well as gram-positive anaerobic Pepto streptococcus and microaerophilic streptococci, are the most common anaerobic bacteria found in lung abscesses.
Staphylococcus aureus, including methicillin-resistant Staphylococcus aureus (MRSA), Streptococcus pneumoniae, Klebsiella pneumonia, Pseudomonas aeruginosa, Haemophilus influenza (type B), Acinetobacter spp., Escherichia coli, and Legionella are the most common isolates from aerobic bacteria found in lung abscesses.
Children's Lung Abscess Pathogen:
- Mycobacterium spp.
- Aspergillus
- Cryptococcus
- Histoplasma
- Blastomyces
- Coccidiosis
- Entamoeba histolytica
- Parasomnias Westermann
Are additional potential etiologic pathogens for lung abscesses. Important etiologic bacteria of lung abscess, Actinomyces and Nocardia asteroids, are known to require a prolonged course of antibiotic treatment (6 months).
There are no patterns for haematological dissemination of lung abscesses, which are etiologically confined in the posterior portions of the lungs after oropharyngeal aspiration.
Diagnosis
The apical segment of the right and occasionally the left lower lobe, the lateral part of the posterior segment of the right upper lobe—the axillary sub segment, and the middle lobe in cases of vomiting and aspiration in the prone position have all been identified as predictors of lung abscess. These conditions are typically associated with alcoholics. They are seen in the posterior portion of the right upper lobe or the apical region of both lungs’ lower lobes in 75% of all lung abscesses.
A pyopneumothorax or pleural empyema will form if the visceral pleura is affected by the infected lung tissue. If the patient is receiving adequate antibiotic treatment and has a strong immune system, the chronic inflammatory response will stop the progression of the disease. Sepsis may develop in cases of inadequate or delayed antibiotic therapy or poor patient general health. Necrotic debris will empty the abscesses cavity if there is a connection to the bronchus, and a radiological indicator of air-fluid level will appear.
- In case of favourable outcome, a necrotic tissue will be eliminated by lysis and phagocytosis and granulation tissue will make a scar tissue.
- If there is a bad outcome, infection may spread throughout the lung tissue and a pleural, mediastinal, or cutaneous fistula may form. In a persistent abscess, fibrosis and calcification can happen in addition to the normal reabsorption of necrotic debris.
- Chest X-ray: This reveals to your doctor the location of the abscess.
- A chest CT scan: Your doctor is searching for a cavity in the middle of your lung that is filled with fluid and air.
- Sputum or lung tissue samples for additional tests using a bronchoscope, a narrow tube with a light and a camera at the end
Therapy
Clindamycin (600 mg IV over 8 hours) is the go-to conservative treatment option for lung abscesses caused by anaerobic bacteria. Clinical investigations have shown that it performs better than penicillin in terms of response rates, fever duration, and time for putrid sputum to clear up. Because some Fusobacterium and Bacteroides species may manufacture -lactamase, they are penicillin-resistant. Penicillin is only effective against about 15-20% of the anaerobic bacteria that cause lung abscesses; hence, combinations with clavulanate or metronidazole are other options.
Due to the presence of many bacteria, most likely microaerophilic streptococci like Streptococcus miller, metronidazole as a single medication does not seem to be very successful.
Combinations of beta-lactam antibiotics with inhibitors of beta-lactamase (ticarcillin-clavulanate, ampicillin-sulbactam, amoxicillin-clavulanate, piperacillin-tazobactam), chloramphenicol, imipenem, or meropenem, second-generation cephalosporins (cefoxitin, cefotetan), and newer-generation fluoroquinolones.
Treatment Response:
Clinical improvements with fever typically manifest within three to four days after taking antibiotics should erupt in 7–10 days. Beyond this point, persistent fevers suggest a delayed response, and such patients should undergo additional diagnostic procedures to identify the underlying anatomy and microbiology of the infection.
Therapeutic response that was delayed Consider:
incorrect microbiological diagnosis obstruction by alien objects or neoplasm larger than 6 cm in diameter, which could necessitate particularly extended treatment times or empyema it calls for drainage Causes that are not infectious: pulmonary infarcts
Due to the polymicrobial flora,
- it is advised to use broad-spectrum antibiotics to treat lung abscesses, such as Clindamycin (600 mg IV on 8 hours, followed by 300 mg PO on 8 hours) or a combination of ampicillin/sulbactam (1.5-3 gr IV on 6 hours).
- Other treatments include Meropenem 1 gr IV for 8 hours or piperacillin/tazobactam 3.375 gr IV for 6 hours.
- Vancomycin 15 mg/kg BM or linezolid 600 mg IV every 12 hours are suggested treatments for MRSA.
- The effectiveness of antibiotic therapy can be observed after three to four days, and the general state of the patient will improve after seven to ten days. However, full healing and radiographic normalization can only be observed after two months.
- The patient's clinical and radiographic response will determine how long the patient receives antibiotic therapy. The duration of antibiotic therapy should be at least as long as the fever, foul sputum, and abscess fluid have subsided; this usually takes between 5 and 21 days for intravenous antibiotic administration and then between 28 and 48 days for oral antibiotic administration with frequent radiographic and laboratory monitoring. Impact of antibiotic treatment on lung abscess radiographic findings.
Percutaneous
Less than 10% of lung abscesses do not respond to antibiotic therapy, thus drainage may be required. If there has been no progress after taking antibiotics for 10 to 14 days, this is typically taken into account.
Drainage can be carried out either by inserting a needle into the abscess via the chest wall (percutaneous drainage) or by using a bronchoscopy and endobronchial ultrasonography (endobronchial drainage). When there is a chance of puncturing lung tissue from central abscesses that are distant from the pleura, endobronchial drainage may be preferred; nonetheless, percutaneous drainage is more frequently used.
- Avoid passive smoking and stop smoking. Smoking harms your lungs and increases your risk of contracting an illness.
- Before eating, before handling food, and after using the lavatory, wash your hands with soap and water. Use a hand sanitizer with alcohol as a substitute for soap.
- If either of you has an infectious sickness like the flu, a cold, or COVID-19, avoid being in close contact with each other and refrain from exchanging things.
- Do not be hesitant to question your healthcare professionals how to lower your risk of contracting an infection while you are a patient in a hospital or other healthcare facility if you must stay there.
- Exercise, maintain a nutritious diet, and get enough sleep.
- Get any further infections or medical issues handled.
Prognosis
The prognosis of a lung abscess depends frequently on the underlying cause with prompt antibiotic treatment, and many lung abscesses clear up without causing any lasting issues.
A lung abscess should be identified and treated right away to lower the risk of consequences.
The answer to many illnesses is prevention. You may lessen your risk by practising good dental hygiene, getting help right away if you think you have pneumonia, managing your airways, and carefully controlling your blood sugar levels if you have diabetes.
- Huge cavities (greater than 6 cm)
- Older age
- Pneumonia with necrosis
- Persistent symptoms
- Abscess brought on by hospital-acquired aerobic bacteria
- Blockage of the bronchi owing to tumours or a foreign object (secondary abscess)
- People with weak immunity









