In addition to the gastrointestinal tract, Crohn's disease and ulcerative colitis have many extraintestinal manifestations. In most patients he can distinguish the disorders, but in at least 10% of patients the features...
Introduction
Recurrent episodes of inflammation characterized the condition known as "inflammatory bowel disease" (IBD). Produced by abnormal immunological reactions to the intestinal flora in the digestive system.
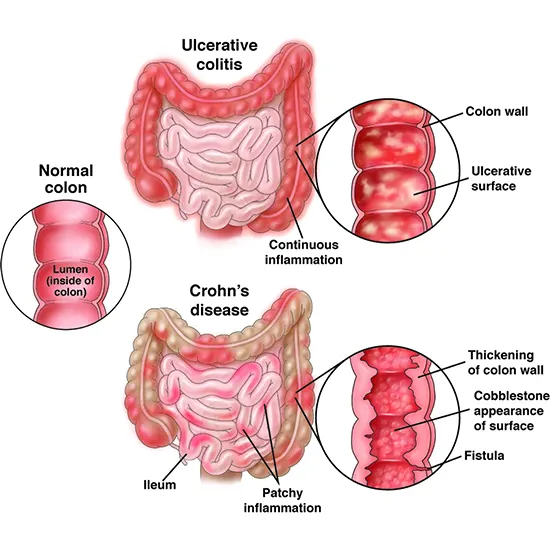
Inflammatory bowel disease consists of two types of idiopathic bowel disease that are distinguished by the location and depth of involvement in the bowel wall. Ulcerative colitis (UC) is a diffuse inflammation of the lining of the colon.
Ulcerative colitis most commonly affects the rectum (proctitis), but can also extend into the sigmoid colon (rectosigmoiditis) and extend beyond the sigmoid colon (distant sigmoiditis). (colonic ulcerative colitis), which can extend from the entire colon to the cecum (pancolitis).
Crohn's disease (CD) causes transmural ulcers in any part of the gastrointestinal (GI) tract, most commonly affecting the terminal ileum and colon. Both diseases are classified by degree (mild, moderate, severe) and location. CDs are also classified by inflammatory, contractile, or penetrant phenotypes.
In addition to the gastrointestinal tract, Crohn's disease and ulcerative colitis have many extraintestinal manifestations. In most patients he can distinguish the disorders, but in at least 10% of patients the features are so similar that he is initially unable to distinguish between the two disorders.
Both disorders have a genetic predisposition. Neither is curable, and both carry enormous morbidity. After all, both increase the risk of colon cancer.
Examination
After an unsuitable immune reaction against the intestinal flora, inflammatory bowel disease (IBD) manifests in people with hereditary susceptibility.
To this day, the cause of IBD remains a mystery. Many causes are involved, but none are common to all patients. One consistent feature of Crohn's disease is its strong association with tobacco. Smoking, on the other hand, appears to protect against ulcerative colitis. The function of diet is still debatable.
Although the CARD15 gene has been linked to IBD, its polymorphism nature makes it impossible to pinpoint which region of the gastrointestinal tract is impacted. There is not a significant genetic component to ulcerative colitis in Crohn's disease.
Epidemiology
In North America, the prevalence of inflammatory bowel disease (IBD) varies from 2.2 to 19.2 cases per 100,000 person-years for ulcerative colitis and 3.1 to 20.2 cases per 200,000 person-years for CD. The prevalence of ulcerative colitis in US adults was 238 per 100,000 population and 201 per 100,000 populations, based on data from large claimed studies.
In comparison to Asia and Africa, North America and Europe have higher rates of IBD. Most IBD occurs in people between the ages of 15 and 30, but up to 25% of people develop IBD during puberty.
Women are slightly more likely than men to have Crohn's disease, but ulcerative colitis appears to be equally common in men and women. IBD is a disease commonly found in developed and cold climates.
Pathophysiology
Inflammatory bowel disease is largely caused by the intestinal immune system (IBD). The intestinal epithelium prevents bacteria and antigens from entering the blood circulation through sealed intercellular junctions. In IBD, these connections are defective as a result of impaired primary barrier function or severe inflammation.
Goblet cells' mucus production and the secretion of -defenses with inherent antibacterial activity by Paneth cells are two additional defensive mechanisms. Excessive inflammatory response leads to continued deterioration of the epithelium and further exposure to gut microbes, further exacerbating inflammation.
In ulcerative colitis, there is constant inflammation of the mucous membranes, causing edema, ulceration, bleeding, and loss of electrolytes. Inflammation in ulcerative colitis usually begins in the rectum and progresses seamlessly to the proximal colon. In Crohn's disease, there are skip lesions.
In nearly 20% of patients with ulcerative colitis, the disease remains confined to the rectum. As the disorder becomes chronic, the colon becomes stiffer and shorter and loses its perforation marks, resulting in the appearance of a lead tube with a barium enema.
The disease can cause strictures, inflammation, or the development of fistulas. The main feature of Crohn's disease is that all layers of the intestine are affected (transmural). In later stages of the disease, the mucosa takes on a cobblestone appearance with linear ulcers between normal mucosa.
Crohn's disease most commonly affects the colon and ileum, with only 5% of cases involving the gastroduodenal segment. Although rectal sparing is typical of Crohn's disease, anorectal complications such as fistulas and abscesses are very common.
Ulcerative colitis predisposes patients to extraintestinal lesions of the skin, eyes, and bones. The most common are inflammatory arthritis and primary sclerosing cholangitis. CD mainly impacts the colon and ileum, although it can also involve the esophagus, duodenum, or stomach.
Childhood-onset cases demonstrate greater involvement of the upper gastrointestinal tract. In the same way that UC does, CD puts patients at risk for extraintestinal symptoms such arthritis, aphthous stomatitis, uveitis, erythema nodosum, and ankylosing spondyloarthropathy.
In Crohn's disease, malabsorption of bile salts and fatty acids increases the incidence of kidney disease and gallstones. Patients with Crohn's disease who have had an ileum resection but an intact colon are also more likely to develop calcium oxalate kidney stones.
Histopathology
Patients with active inflammatory bowel disease (IBD) exhibit substantial lamina propria infiltration by a combination of neutrophils, macrophages, dendritic cells, and natural killer T cells. Increased numbers and activation of these cells increase levels of cytokines in the tumor necrosis factor-a (TNF-a), interleukin-1b, interferon-gamma, and interleukin-23-TH17 signaling pathways.
Histopathology of ulcerative colitis shows that only the mucosa and submucosa are involved in the formation of occult abscesses and mucosal ulcers. Biopsy specimens show neutrophilic infiltration with crypt distortion and crypt abscesses. In ulcerative colitis, there are no granulomas. These illnesses frequently affect the rectum and are connected.
Pseudopolyps are another defining feature of ulcerative colitis. In Crohn's disease, the entire intestinal wall is affected and granulomas may be seen. Inflammation in Crohn's disease is transmural and characterized by lymphocytic infiltration.
History and Physical
Bloody diarrhoea, with or without mucous, is the most typical symptom of ulcerative colitis. Patients usually complain of tenesmus, incomplete evacuation, and abdominal pain. A physical examination may show abdominal pain, primarily in the lower left or upper left quadrant. Signs of acute abdomen such as guard, rebound, or percussion warrant evaluation for toxic megacolon.
Symptoms of Crohn's disease vary greatly depending on the area of the gastrointestinal tract involved. Depending on the underlying cause of the inflammation, fistula formation, or stricture creation, different symptoms will manifest.
A combination of pain in the right lower quadrant, weight loss, and bloodless diarrhea suggest relapse of Crohn's disease. Fistula formation can lead to fecal enuresis, pneumonia, and rectovaginal fistula. A mass in the lower right abdomen suggests an abscess. Affected children may exhibit growth retardation and delayed sexual maturity.
World Gastroenterology Society based on her IBD symptoms
- Diarrhea may be accompanied by blood or mucus. Diarrhea can also occur at night and fecal incontinence is not uncommon.
- Some people with ulcerative colitis may experience constipation if the disease is confined to the rectum.
- Abdominal pain, tenesmus, and a strong urge to urinate are also common symptoms.
- Crohn's disease presents with right lower quadrant pain, ulcerative colitis with left lower quadrant pain.
- Nausea and vomiting are more common in Crohn's disease.
Physical Examination
-
Pallor may be noted in some anemia.
- Toxic megacolon can cause severe pain, fever, bloating, chills, and lethargy. This surgical emergency can be fatal if missed and should always be considered. In Crohn's disease, anal fistulas, abscesses, and even rectal prolapse may be seen.
- Occult blood on digital rectal examination is common.
- Only growth retardation is observed in children.
Evaluation
Clinical signs, inflammatory laboratory markers, imaging findings, and endoscopic biopsy must all be considered in the diagnosis of inflammatory bowel disease (IBD).
Hematological findings include microcytic anemia, leukocytosis and thrombocytosis, and high-sensitivity and erythrocyte sedimentation rate (ESR) are examples of inflammatory indicators C-reactive protein (hsCRP) are often elevated.
In some patients, diagnosis may require exclusion of prevalence such as giardiasis, amebiasis, nematosis, and tuberculosis. A complete blood count identifies anemia, leukocytosis, and albumin levels.
Fecal calprotectin levels can be used as a marker of intestinal inflammation. Perinuclear anti-neutrophil cytoplasmic and anti-Saccharomyces cerevisiae antibody levels may be elevated in Crohn's disease. Finally, a stool test should be performed to rule out eggs or parasites.
Abdominal X-rays can assess the presence of empty air, intestinal obstruction, or toxic megacolon.
A barium study is done to characterize bowel disease. The appearance of lead pipes indicates ulcerative colitis. Sparing the rectum indicates Crohn's disease and the thumbprint indicates inflammation of the mucosa. In addition, barium studies may reveal ileal skip lesions and stricture formation indicative of Crohn's disease.
IBD can be diagnosed or its complications evaluated using ultrasound, computed tomography, or magnetic resonance imaging (MRI). The US application for trained individuals can examine the right lower quadrant for ileal disease. MRI can assess rectal fistula. Most commonly, CT is used to check for perforation or bowel obstruction. CT bowel graph can help evaluate strictures and plan surgery.
Treatment/Management
The goal of treatment is to induce remission of UC or CD. Treatment of IBD is divided into treatment of mild, moderate and severe disease. Means reserved for more serious illnesses are now used earlier. The condition's severity and the presence of extraintestinal symptoms greatly influence how ulcerative colitis should be treated.
For mild to moderate disease confined to the rectum, aminosalicylic acids like mesalamine are the mainstays. Mesalamine is given rectally but can be combined with oral therapy to induce or maintain remission.
Immunomodulatory agents such as oral glucocorticoids or TNF-alpha monoclonal antibody (infliximab) may be an option for patients with moderate disease who are resistant to mescaline. Up to 25% of all UC patients will require a total colectomy due to uncontrolled disease. [9][10][11] In elective cases, proctocolectomy (IPAA) with pouch-anal anastomosis is the procedure of choice.
Relapses are usually treated with corticosteroid therapy. Anti-TNF or other immunosuppressive agents are recommended for relapses more than 1-2 times a year.
Treatment of CD depends on the portion of the GI tract affected, the degree of fistula formation or stricture, and extraintestinal complications. Treatment of mild ileocecal disease is usually initiated with mesalamine, which is further augmented with oral budesonide, a steroid with significant first-pass metabolism, to limit systemic side effects.
The more extensive disease requires systemic steroid therapy with prednisone. The goal is for him to stop using these steroids within six weeks. Immunomodulators such as 6-mercaptopurine, azathioprine, or low-dose methotrexate are added in non-weaning patients.
Anti-tumor necrosis factor (anti-TNF) therapy should be initiated in patients with moderate to severe disease. Before starting biologic therapy, patients should undergo a purified protein derivative (PPD) test to detect latent tuberculosis. [1][12][13] Patients with severe fistulizing disease, including bypass ostomy, may require surgical treatment.
It is important to assess bone density in patients receiving steroids. Osteoporosis poses significant morbidity in these patients. If steroid use he anticipates for more than 3 months, calcium supplements and bisphosphonates should be started.
Differential Diagnosis
Infectious etiology of diarrhea, including the parasite, E. coli 0157, in patients presenting with diarrhea:
- H7 and Clostridium difficile should be excluded first. Additional colitis aetiologies, such as microscopic, lymphocytic, and collagenous, should be taken into account.
- Other causes such as appendicitis, irritable bowel disease, celiac disease, and functional abdominal pain should also be considered in patients with abdominal pain.
Prognosis
The prognosis for UC and MC depends on the extent of disease and response to treatment. The stool markers lactoferrin and calprotectin help determine postoperative recurrence of MC. There is evidence to support their use in eruption forecasting.
However, IBD patients tend to have a much higher mortality rate compared to the general population. Causes of death are primary disease, infection, and respiratory disease. Heart disease is not a risk factor for his dying from IBD. Finally, IBD patients have very high psychiatric morbidity and poor quality of life.
Continuous monitoring of dysplasia is critical for long-standing UC patients. Those over the age of 30 are thought to have a cumulative risk of up to 30% for colorectal cancer.
Extraintestinal manifestations of primary sclerosing cholangitis lead to liver failure.
Complications
Complications of inflammatory bowel disease (IBD) fall into her two categories: intestinal and extraintestinal.
Intestinal
- Bleeding
- Limit
- Colonic perforation
- Anal fistula
- Pelvic or perirectal abscess
- Poisonous megacolon
- Bile duct cancer, colon cancer
- Extraintestinal
Extraintestinal
- Osteoporosis
- Deep vein thrombosis
- Anemia
- Gallstones
- Primary sclerosing cholangitis
- Aphthous ulcer
- Arthritis
- Iritis
- Pyoderma gangrenosum









