Azotemia is a condition in which there is a buildup of nitrogenous waste products, such as urea and creatinine, in the blood. These waste products are normally excreted from the body through the urine, but in azotemia, the...
"Clearing the cloud of nitrogenous waste: Understanding and managing azotemia."
An Overview
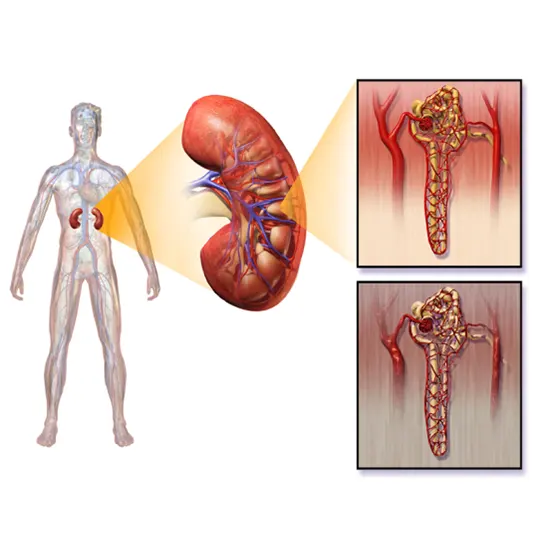
Azotemia is a condition in which there is a buildup of nitrogenous waste products, such as urea and creatinine, in the blood. These waste products are normally excreted from the body through the urine, but in azotemia, the kidneys are not functioning properly and are unable to remove them from the blood efficiently.
Azotemia can be caused by a variety of factors, including dehydration, kidney disease, heart failure, liver disease, and certain medications that can be toxic to the kidneys. Acute kidney injury (AKI) and chronic kidney disease (CKD) are the most common causes of azotemia.
AKI is a sudden and often reversible decline in kidney function that can be caused by factors such as dehydration, infections, medications, and toxins. It can lead to azotemia if the kidneys are unable to remove nitrogenous waste products from the blood. CKD, on the other hand, is a chronic condition in which the kidneys gradually lose their function over time. As CKD progresses, the buildup of nitrogenous waste products in the blood can lead to azotemia.
A Silent yet Serious Threat - Commonness of Azotemia
Azotemia is a relatively common condition, especially among older adults and those with pre-existing kidney disease or other health conditions that affect kidney function. However, the prevalence of azotemia varies depending on the underlying cause of the condition and the population being studied.
According to a study published in the Journal of Hospital Medicine, the prevalence of azotemia among hospitalized patients in the United States is around 10-20%, with higher rates observed in older adults and those with comorbid conditions.
Azotemia is a common condition in India too and is often associated with chronic kidney disease (CKD), which is a significant health problem in the country. According to a study published in the Indian Journal of Nephrology, the prevalence of CKD in India is estimated to be around 8-17% in the general population. CKD is a major risk factor for azotemia, and patients with CKD are at a higher risk of developing azotemia.
Azotemia is on the rise: Know the Causes and preserve kidney health
Some of the common causes of azotemia include:
- Kidney disease: Azotemia is most commonly associated with kidney disease, including acute kidney injury (AKI) and chronic kidney disease (CKD). In these conditions, the kidneys may not be able to filter waste products effectively, leading to a buildup of nitrogenous waste in the blood.
- Dehydration: When the body is dehydrated, the kidneys may struggle to eliminate waste products effectively, leading to an increased risk of azotemia.
- Medications: Certain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), angiotensin-converting enzyme (ACE) inhibitors, and some antibiotics, can cause kidney damage and impair kidney function, increasing the risk of azotemia.
- Urinary tract obstruction: Blockages in the urinary tract, such as kidney stones or an enlarged prostate gland, can cause urine to back up into the kidneys, impairing their function and increasing the risk of azotemia
- Infections: Certain infections, such as pyelonephritis (a type of kidney infection) and sepsis (a life-threatening infection), can damage the kidneys and impair their function, leading to azotemia.
- Shock: Severe shocks, such as that caused by a major injury or blood loss, can reduce blood flow to the kidneys, impairing their function and increasing the risk of azotemia.
It's important to note that the underlying cause of azotemia may not always be apparent, and prompt diagnosis and treatment are essential to prevent complications and improve outcomes.
Understanding the root cause: Delving into the pathogenesis of azotemia
The pathogenesis of azotemia can be understood in the following way:
- Impaired kidney function: In most cases, azotemia occurs as a result of impaired kidney function. The kidneys are responsible for filtering waste products from the blood and excreting them in urine. If the kidneys are unable to perform this function effectively, due to damage or disease, nitrogenous waste products can build up in the blood, leading to azotemia.
- Increased production of nitrogenous waste: In some cases, azotemia can occur even when kidney function is normal. This can happen when there is an increased production of nitrogenous waste products, such as urea and creatinine, due to factors such as high protein intake or increased catabolism (breakdown) of protein in the body.
- Reduced blood flow to the kidneys: In some cases, reduced blood flow to the kidneys, known as renal hypoperfusion, can impair kidney function and lead to azotemia. This can occur in conditions such as shock or severe dehydration.
- Obstruction of the urinary tract: Obstruction of the urinary tract, such as by kidney stones or an enlarged prostate gland, can cause urine to back up into the kidneys, impairing their function and leading to azotemia.
- Direct kidney damage: In some cases, direct damage to the kidneys, such as from an infection or medication toxicity, can impair their function and lead to azotemia.
Overall, the pathogenesis of azotemia is complex and can involve multiple factors. Prompt diagnosis and treatment of underlying conditions that affect kidney function are essential to prevent complications and improve outcomes.
Recognize the Signs and Symptoms of Azotemia
Azotemia may not cause any symptoms in its early stages, but as the condition progresses and levels of nitrogenous waste products in the blood continue to rise, several signs and symptoms may appear. Some of the common signs and symptoms of azotemia include:
- Fatigue and weakness: Elevated levels of nitrogenous waste products in the blood can cause fatigue and weakness, making it difficult to perform daily activities.
- Decreased urine output: In some cases, azotemia can cause a decrease in urine output or a complete absence of urine production. This can be a sign of severe kidney damage and requires immediate medical attention.
- Nausea and vomiting: Elevated levels of nitrogenous waste products in the blood can cause nausea and vomiting, particularly in cases where kidney function is severely impaired.
- Loss of appetite: Azotemia can cause a loss of appetite or an aversion to certain foods, particularly those high in protein
- Swelling: Fluid retention can occur in people with azotemia, leading to swelling in the legs, feet, and ankles.
- Confusion and difficulty concentrating: Elevated levels of nitrogenous waste products in the blood can affect brain function, leading to confusion, difficulty concentrating, and memory problems.
- Shortness of breath: In severe cases, azotemia can cause shortness of breath and difficulty breathing, particularly during physical activity.
It's important to note that the symptoms of azotemia can vary depending on the underlying cause and severity of the condition. Prompt diagnosis and treatment are essential to prevent complications and improve outcomes.
Early Detection is Key: The diagnostic tests to determine azotemia
The diagnosis of azotemia typically involves a combination of clinical tests, laboratory tests, and radiographic imaging. Here are some of the common diagnostic tests used to evaluate azotemia:
Clinical tests:
Clinical tests involve a physical examination and assessment of the patient's symptoms. Some common clinical tests used to evaluate azotemia include:
- Blood pressure measurement: Elevated blood pressure can be a sign of kidney disease.
- Urinalysis: This test can detect the presence of protein, blood, or other abnormal substances in the urine
- Fluid intake and output measurement: Measuring the volume of fluids taken in and excreted can help assess kidney function.
Laboratory tests:
Laboratory tests help to evaluate the level of nitrogenous waste products in the blood and urine. Some common laboratory tests used to evaluate azotemia include:
- Blood urea nitrogen (BUN) test: The amount of nitrogen in the blood that comes from the breakdown of urea is measured. Raised BUN levels may indicate kidney dysfunction.
- Creatinine test: The level of creatinine in the blood is measured. Creatinine is a waste product produced by muscle metabolism and is filtered out of the blood by the kidneys. Heightened creatinine levels may indicate kidney dysfunction.
- Electrolyte panel: The levels of various electrolytes in the blood, such as sodium, potassium, and chloride are calculated. Electrolyte imbalances can be a sign of kidney dysfunction.
- Glomerular filtration rate (GFR): It is an important diagnostic tool used to evaluate azotemia. Azotemia is often caused by a decrease in GFR, which results in the accumulation of nitrogenous waste products in the blood.
GFR is a measure of the rate at which blood is filtered through the kidneys. It is calculated based on the level of creatinine in the blood, which is a waste product produced by muscle metabolism. The GFR is calculated using a formula that takes into account the patient's age, gender, and race. A GFR below 60 mL/min/1.73m² is considered a sign of kidney dysfunction.
Radiographic Tests
Radiographic imaging tests help to evaluate the structure and function of the kidneys. Some common radiographic tests used to evaluate azotemia include:
- Ultrasound: The images of the kidneys and urinary tract are created using sound waves.
- CT scan: Detailed images of the kidneys and urinary tract are created using computer technology.
- MRI: Uses a magnetic field and radio waves to create detailed images of the kidneys and urinary tract.
Overall, a combination of these tests can be used to diagnose and evaluate the severity of azotemia and to determine the underlying cause of the condition.
From medication to surgery: Exploring the treatment options for azotemia.
Treatment options for azotemia depend on the underlying cause and severity of the condition.
Medications
Medications are often used to treat azotemia caused by kidney dysfunction. Some common medications include:
- Diuretics: These medications increase urine output and can help reduce the amount of nitrogen-containing compounds in the blood.
- ACE inhibitors and ARBs: These medications are used to treat high blood pressure and can also help protect the kidneys from further damage.
- Erythropoietin: This medication stimulates the production of red blood cells and can help treat anemia, which is a common complication of kidney dysfunction.
- Phosphate binders: These medications help reduce the amount of phosphate in the blood and can be used to treat hyperphosphatemia, which is a common complication of kidney dysfunction.
Surgical Options
In some cases, surgical intervention may be necessary to treat azotemia. Examples of surgical interventions include:
- Dialysis: This is a medical procedure that involves using a machine to filter the blood and remove excess nitrogen-containing compounds. Dialysis is often used to treat severe cases of azotemia caused by kidney dysfunction.
- Kidney transplant: This surgical procedure involves replacing a diseased or damaged kidney with a healthy donor kidney. A kidney transplant is often considered the best option for treating azotemia caused by irreversible kidney damage.
- Surgery to remove an obstruction: If azotemia is caused by a urinary tract obstruction, surgery may be necessary to remove the obstruction and restore normal urine flow.
- Nephrectomy: This is a surgical procedure that involves removing a diseased or damaged kidney. Nephrectomy may be necessary if one kidney is significantly damaged and causing azotemia, and the other kidney is healthy enough to maintain normal kidney function.
It is important to note that the treatment of azotemia should be individualized based on the underlying cause and severity of the condition. Patients should work closely with their healthcare providers to determine the most appropriate treatment plan.
Handle with care: Essential precautions for individuals living with azotemia.
When someone has azotemia, certain things should be avoided to prevent further damage to the kidneys and to improve overall health. Here are some things to avoid during azotemia:
- Dehydration: Dehydration can worsen azotemia by reducing urine output and increasing the concentration of nitrogen-containing compounds in the blood. Therefore, it is important to drink plenty of water and other fluids to stay hydrated.
- High-protein diets: High-protein diets can increase the workload on the kidneys and lead to an accumulation of nitrogen-containing compounds in the blood. Therefore, it is best to limit protein intake during azotemia.
- Alcohol and tobacco: Both alcohol and tobacco can be harmful to the kidneys and can worsen azotemia. Therefore, it is important to avoid alcohol and tobacco during azotemia.
- Certain medications: Some medications can be harmful to the kidneys and can worsen azotemia. Patients should talk to their healthcare provider about any medications they are taking to determine if any changes need to be made.
- Over-the-counter supplements: Some over-the-counter supplements, such as creatine, can increase the workload on the kidneys and lead to an accumulation of nitrogen-containing compounds in the blood. Therefore, it is best to avoid these supplements during azotemia.
" Fight back against azotemia, Don't let it scare you down"









